Angiogenic Factors Serum Level Variations in Pregnancy with Chronic Arterial Hypertension
The aim of the investigation was to study the change of vascular growth factors in physiological pregnancy, and pregnancy with chronic arterial hypertension.
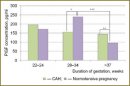
Materials and Methods. We carried out a detailed clinical analysis of the gestation course of 69 pregnant women with chronic arterial hypertension, and 49 women with normal pregnancy. All women underwent dynamic study of pro-angiogenic (PlGF) and anti-angiogenic (sFlt-1, endoglin) factor levels in blood serum on the 22–24, 28–34 weeks and after the 37 week of gestation.
Results. In complicated pregnancy the level of pro- and anti-angiogenic factors on the 22–24 weeks of gestation was no different from a normal level, on the 28–34 weeks there was the increase of concentration of anti-angiogenic sFlt-1 up to 5573±774 pg/ml (in control — 3299±544 pg/ml, p<0.001), and endoglin — up to 7.1±0.8 ng/ml (in control — 5.4±0.4 ng/ml, p<0.001). Simultaneously there was the decrease of pro-angiogenic PlGF (155.8±30.4 v. 238.5±66.1 pg/ml in control, p<0.05). On the 37 week of gestation the sFlt-1 level grew in both abnormal pregnancy, and normal pregnancy (13334±909 and 13298±740 pg/ml, respectively), while PlGF amount decreased (144.4±81.4 and 94.5±78.2 pg/ml, respectively, p<0.01).
Conclusion. In the third trimester of pregnancy there is the change of angiogenic factors balance in blood serum in pregnant women with chronic arterial hypertension consisting in the increase of anti-angiogenic sFlt-1 and endoglin and the decrease of pro-angiogenic PlGF compared to the norm; it can indicate the abnormality of placentation processes.
- Sibai B.M. Diagnosis, prevention, and management of eclampsia. Obstet Gynecol 2005; 105(2): 402–410.
- Tokova Z.Z. Statisticheskie aspekty gipertenzivnykh rasstroystv vo vremya beremennosti, rodov i v poslerodovom periode. V kn.: Materialy VI Rossiyskogo foruma «Mat’ i ditya» [Statistical aspects of hypertensive disorders in pregnancy, labors, and puerperal period. In: Proceedings of VI Russian Forum “Mother and Child”]. Moscow; 2004; p. 645.
- Duley L. Pre-eclampsia and hypertension. Clin Evid 2004; 12: 2016–2034.
- Zhang J., Meikle S., Trumble A. Severe maternal morbidity associated with hypertensive disorders in pregnancy in the United States. Hypertens Pregnancy 2003; 22(2): 203–212.
- Sukhikh G.T., Murashko L.E. Preeklampsiya [Preeclampsy]. Moscow: GEOTAR-Media; 2010; 576 p.
- Kiefer F.N., Neysari S., Humar R., Li W., Munk V.C., Battegay E.J. Hypertension and angiogenesis. Curr Pharm Des 2003; 9(21): 1733–1744.
- Feihl F., Liaudet L., Waeber B., Levy B.I. Hypertension: a disease of the microcirculation? Hypertension 2006; 48(6): 1012–1017.
- Loomans C.J., Dao H.H., van Zonneveld A.J., Rabelink T.J. Is endothelial progenitor cell dysfunction involved in altered angiogenic processes in patients with hypertension? Curr Hypertens Rep 2004; 6(1): 51–54.
- Debbabi H., Uzan L., Mourad J.J., Safar M., Levy B.I., Tibirica E., Increased skin capillary density in treated essential hypertensive patients. Am J Hypertens 2006; 19(5): 477–483.
- Levy B.I., Ambrosio G., Pries A.R., Struijker-Boudier H.A. Microcirculation in hypertension: a new target for treatment? Circulation 2001; 104(6): 735–740.
- Serne E.H., Gans R.O., ter Maaten J.C., Tangelder G.J., Donker A.J., Stehouwer C.D. Impaired skin capillary recruitment in essential hypertension is caused by both functional and structural capillary rarefaction. Hypertension 2001; 38(2): 238–242.
- Roodink I., Leenders W.P. Targeted therapies of cancer: angiogenesis inhibition seems not enough. Cancer Lett 2010; 299(1): 1–10.
- Solomon C.G., Seely E.W. Preeclampsia — searching for the cause. N Engl J Med 2004; 350(7): 641–642.
- Makris A., Thornton C., Thompson J., Thomson S., Martin R., Ogle R., Waugh R., McKenzie P., Kirwan P., Hennessy A. Uteroplacental ischemia results in proteinuric hypertension and elevated sFLT-1. Kidney Int 2007; 71(10): 977–984.
- Redecha P., van Rooijen N., Torry D., Girardi G. Pravastatin prevents miscarriages in mice: role of tissue factor in placental and fetal injury. Blood 2009; 113(17): 4101–4109.
- Wallner W., Sengenberger R., Strick R., Strissel P.L., Meurer B., Beckmann M.W., Schlembach D. Angiogenic growth factors in maternal and fetal serum in pregnancies complicated by intrauterine growth restriction. Clin Sci (Lond) 2007; 112(1): 51–57.
- Andraweera P.H., Dekker G.A., Roberts C.T. The vascular endothelial growth factor family in adverse pregnancy outcomes. Hum Reprod Update 2012; 18(4): 436–457.
- Aggarwal P.K., Chandel N., Jain V., Jha V. The relationship between circulating endothelin-1, soluble fms-like tyrosine kinase-1 and soluble endoglin in preeclampsia. J Hum Hypertens 2012; 26(4): 236–241.
- Verlohren S., Stepan H., Dechend R. Angiogenic growth factors in the diagnosis and prediction of pre-eclampsia. Clin Sci (Lond) 2012; 122(2): 43–52.
- Masuyama H., Segawa T., Sumida Y., Masumoto A., Inoue S., Akahori Y., Hiramatsu Y. Different profiles of circulating angiogenic factors and adipocytokines between early- and late-onset pre-eclampsia. BJOG 2010; 117(3): 314–320.
- Baeten J.M., Bukusi E.A., Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health 2001; 91(3): 436–440.
- Fortner R.T., Pekow P., Solomon C.G., Markenson G., Chasan-Taber L. Prepregnancy body mass index, gestational weight gain, and risk of hypertensive pregnancy among Latina women. Am J Obstet Gynecol 2009; 200(2): 167.e1-7. doi: 10.1016/j.ajog.2008.08.021.
- Brown M.A., Lindheimer M.D., de Swiet M., Van Assche A., Moutquin J.M. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001; 20(1): IX–XIV.
- Verlohren S., Herraiz I., Lapaire O., Schlembach D., Moertl M., Zeisler H., Calda P., Holzgreve W., Galindo A., Engels T., Denk B., Stepan H., The sFlt-1/PlGF ratio in different types of hypertensive pregnancy disorders and its prognostic potential in preeclamptic patients. Am J Obstet Gynecol 2012; 206(1): 58.e1-8. doi: 10.1016/j.ajog.2011.07.037.










