Therapeutic Effect Consolidation in Overactive Bladder Treatment in Elderly Women by the Use of Increased Antimuscarinic Dosages
Previously, the authors had carried out the study, in which the patients after trospium hydrochloride course with minimal or unstable therapeutic effect were administered the combination of trospium and an increased dosage of one of three antimuscarinics — oxybutinin, solifenacin and tolterodine for 6 weeks. This combination of drug therapy of elderly women with overactive bladder (OAB) was found to result in stable clinical and urodynamic result causing no additional side effects.
The present study was aimed at searching an optimal supporting course, which would enable to consolidate an initial effect and reduce the risk of OAB recurrence.
The aim of the investigation was to assess the possibilities of improving the supporting therapy efficiency in elderly women with overactive bladder using double doses of trospium hydrochloride and solifenacin.
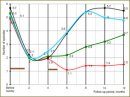
Materials and Methods. The study included 229 women (mean age — 66.3 years: from 65 to 77) with clinically confirmed overactive bladder, who received daily trospium — 60 mg and solifenacin — 40 mg for 6 weeks (such treatment regimen had been justified in the previous study). In order to study the possibilities of each type of supporting therapy, the patients were divided into four groups: group 1 (n=59) was given trospium (60 mg o.d.) + solifenacin (40 mg o.d.) for a month; group 2 (n=51) — detrusor electrical stimulation for a month; group 3 (n=63) — laseropuncture for a month; and group 4 (n=56) patients were given placebo. A supporting therapy course followed the main course 2.5 months later. The patients’ condition was monitored using OAB-q questionnaires (for a year) and urodynamic examination (before a treatment course, 6 and 12 months after the study initiation).
Results. A group of elderly women with OAB underwent a short course of treatment by high (double) doses of two antimuscarinics of different generations (trospium and solifenacin) 2.5 months after the main therapy, which had been similar, and enabled to maintain the initial clinical and urodynamic result for a long period of time (minimum 7 months), with the level of side effects being acceptable. The patients were found to have a high correlation of urodynamic and clinical indices on 6 and 12 month of the study. The use of detrusor electrical stimulation and laseropuncture as a supporting therapy does not enable to maintain a positive effect of drug therapy for a long time.
Conclusion. The supporting course of OAB treatment in elderly women by a combination of high doses of antimuscarinics two months after the main therapy course is the most effective method to reduce the symptomatic relapse risk of the disease.
- De Ridder D., Roumeguere T., Kaufman L. Overactive bladder symptoms, stress urinary incontinence and associated bother in women aged 40 and above; a Belgian epidemiological survey. Int J Clin Pract 2013 Mar; 67(3): 198–204.
- Sexton C.C., Coyne K.S., Thompson C., Bavendam T., Chen C.I., Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older Americans: results from the epidemiology of lower urinary tract symptoms study. J Am Geriatr Soc 2011 Aug; 59(8): 1465–1470.
- Lee Y.S., Lee K.S., Jung J.H., et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol 2011 Apr; 29(2): 185–190.
- Andersson K.E. Muscarinic acetylcholine receptors in the urinary tract. Handb Exp Pharmacol 2011; (202): 319–344.
- Igawa Y., Aizawa N., Homma Y. Beta3-adrenoceptor agonists: possible role in the treatment of overactive bladder. Korean J Urol 2010 Dec; 51(12): 811–818.
- Kanai A.J. Afferent mechanism in the urinary tract. Handb Exp Pharmacol 2011; (202): 171–205.
- Coyne K.S., Payne C., Bhattacharyya S.K., et al. The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: results from a national community survey. Value Health 2004; 7: 455–463.
- Harris C., Smith P.P. Overactive bladder in the older woman. Clinical Geriatrics 2010; 18(09): 41–47.
- Taylor J.A. 3rd, Kuchel G.A. Detrusor underactivity: Clinical features and pathogenesis of an underdiagnosed geriatric condition. J Am Geriatr Soc 2006; 54: 1920–1932.
- Pfisterer M.H., Griffiths D., Schafer W., Resnick N.M. The effect of age on lower urinary tract function: a study in women. J Am Geriatr Soc 2006; 54(3): 405–412.
- Campeau L., Tu L., Lemieux M., et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn 2007; 26: 990–994.
- Chancellor M.B., Anderson R.U., Boone T.B. Pharmacotherapy for neurogenic detrusor overactivity. Am J Phys Med 2006; 85: 536–545.
- Ulahannan D., Wagg A. The safety and efficacy of tolterodine extended release in the treatment of overactive bladder in the elderly. Clin Interv Aging 2009; 4: 191–196.
- Chancellor M.B., Zinner N., Whitmore K., Kobashi K., Snyder J.A., Siami P., Karram M., Laramée C., Capo’ J.P. Jr, Seifeldin R., Forero-Schwanhaeuser S., Nandy I. Efficacy of solifenacin in patients previously treated with tolterodine extended release 4 mg: results of a 12-week, multicenter, open-label, flexible-dose study. Clin Ther 2008 Oct; 30(10): 1766–1781.
- Brostrom S., Hallas J. Persistence of antimuscarinic drug use. Eur J Clin Pharmacol 2009; 65: 309–314.
- Wyndaele J.-J. Conservative treatment of patients with neurogenic bladder. Eur Urol Suppl 2008; 7: 557–565.
- Johnson T.M. II, Burgio K., Redden D., et al. Effects of behavioral and drug therapy on nocturia in older incontinent women. J Am Geriatr Soc 2005; 53: 846–850.
- Korstanje C., Krauwinkel W. Specific pharmacokinetic aspects of the urinary tract. Handb Exp Pharmacol 2011; (202): 267–282.
- Athanasopoulos A. The pharmacotherapy of overactive bladder. Expert Opin Pharmacother 2011 May; 12(7): 1003–1005.
- Madersbacher S., Pycha A., Schatzl G., et al. The aging lower urinary tract: a comparative urodynamic study of men and women. Urology 1998; 51: 206–212.
- Chapple C.R., Khullar V., Gabriel Z., Muston D., Bitoun C.E., Weinstein D. The effects of antimuscarinic treatments in overactive bladder, an update of a systematic review and metaanalysis. Eur Urol 2008; 54: 543–562.
- Amend B., Hennenlotter J., Schäfer T., Horstmann M., Stenzl A., Sievert K.-D. Effective treatment of neurogenic detrusor dysfunction by combined high-dosed antimuscarinics without increased side-effects. Eur Urol 2008; 53: 1021–1028.
- Horstmann M., Schaefer T., Aguilar Y., Stenzl A., Sievert K.D. Neurogenic bladder treatment by doubling the recommended antimuscarinic dosage. Neurourol Urodyn 2006; 25(5): 441–445.
- Kosilov K.V., Loparev S.A., Ivanovskaya M.A., Kosilova L.V. Management of overactive bladder (OAB) in elderly men and women with combined, high-dosed antimuscarinics without increased side effects. UroToday Int J 2013 Aug; 6(4): art 47.
- Ruby C.M., Hanlon J.T., Boudreau R.M., Newman A.B., Simonsick E.M., Shorr R.I., Bauer D.C., Resnick N.M. The effect of medication use on urinary incontinence in community-dwelling elderly women. J Am Geriatr Soc 2010 Sep; 58(9): 1715–1720.
- Chapple C. New once-daily formulation for trospium in overactive bladder. Int J Clin Pract 2010 Oct; 64(11): 1535–1540.
- Wyndaele J.-J., Goldfischer E.R., Morrow J.D., et al. Effects of flexible-dose fesoterodine on overactive bladder symptoms and treatment satisfaction: an open-label study. Int J Clin Pract 2009 Apr; 63(4): 560–567.
- Madersbacher S. Combination therapy of benign prostate syndrome/lower urinary tract symptoms. Urologe A 2013 Feb; 52(2): 212–218.
- Otsuki H., Kosaka T., Nakamura K., Mishima J., Kuwahara Y., Tsukamoto T. β3-Adrenoceptor agonist mirabegron is effective for overactive bladder that is unresponsive to antimuscarinic treatment or is related to benign prostatic hyperplasia in men. Int Urol Nephrol 2013 Feb; 45(1): 53–60.
- Brubaker L. Electrical stimulation in overactive bladder. Urology 2000 May; 55(5A Suppl): 17–23; discussion 31–32.
- Slovak M., Barker A.T., Chapple C.R. The assessment of a novel electrical stimulation waveform recently introduced for the treatment of overactive bladder. Physiol Meas 2013 May; 34(5): 479–486.
- Lewey J., Lilas L. Electrical stimulation of the overactive bladder. Prof Nurse 1999 Dec; 15(3): 211–214.
- Ozdedeli S., Karapolat H., Akkoc Y. Comparison of intravaginal electrical stimulation and trospium hydrochloride in women with overactive bladder syndrome: a randomized controlled study. Clin Rehabil 2010 Apr; 24(4): 342–351.
- Leong F.C., McLennan M.T. Neuromodulation for the treatment of urinary incontinence. Mo Med 2007 Sep–Oct; 104(5): 435–439.
- Bschleipfer T., Lüdecke G., Durschnabel M., Wagenlehner F.M., Weidner W., Pilatz A. Auricular acupuncture in patients with detrusor overactivity: a pilot study. Urologe A 2013 Apr 20. [Epub ahead of print].
- Emmons S.L., Otto L. Acupuncture for overactive bladder: a randomized controlled trial. Obstet Gynecol 2005 Jul; 106(1): 138–143.
- Kitakoji H., Terasaki T., Honjo H., Odahara Y., et al. Effect of acupuncture on the overactive bladder. Nihon Hinyokika Gakkai Zasshi 1995 Oct; 86(10): 1514–1519.
- Tian F.S., Zhang H.R., Li W.D., et al. Study on acupuncture treatment of diabetic neurogenic bladder. Zhongguo Zhen Jiu 2007 Jul; 27(7): 485–487.
- Parsons M., Amundsen C.L., Cardozo L., Vella M., Webster G.D., Coats A.C. Bladder diary patterns in detrusor overactivity and urodynamic stress incontinence. Neurourol Urodyn 2007; 26(6): 800–806.
- Amundsen C.L., Parsons M., Cardozo L., Vella M., Webster G.D., Coats A.C. Bladder diary volume per void measurements in detrusor overactivity. J Urol 2006 Dec; 176(6 Pt 1): 2530–2534.
- Schroder A., Abrams P., Andersson K.-E., et al. Guidelines on urinary incontinence. European Association of Urology 2009; 52 р.
- Woodford H., George J. NICE guidelines on urinary incontinence in women. Age Ageing 2007; 36: 349–50.
- Singh G., Lucas M., Dolan L., Knight S., Ramage C., Hobson P.T. Minimum standards for urodynamic practice in the UK. Neurol Urodyn 2010 Nov; 29(8): 1365–1372.
- Schafer W., Abrams P., Liao L., et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurol Urodyn 2002; 21: 261–274.










