Laser Microablative Tunnel Formation to Initiate Alveolar Bone Regeneration. Pilot ex vivo Study
In recent years there has been demonstrated the ability of Erbium (Er) laser to cause effective ablation of bone tissue with minimum collateral damage. Non-surgical treatment of periodontitis using Er laser improves probing depth and clinical attachment level. However, periodontal anti-inflammatory therapy should not be limited to these parameters, but also should initiate tissue regeneration including bone tissue damaged by the disease.
The aim of the investigation was to evaluate feasibility and characterize the process of laser microablative tunnel formation in gingiva and alveolar bone using a pulse-periodic, single mode Er laser, and determine laser parameters providing appropriate size of the tunnel and coagulation zone needed to initiate healing and regeneration of the alveolar bone.
Materials and Methods. Ex vivo pig jaw was used as a model for the study. To create a through-gingiva microperformation of the alveolar bone, we used a laboratory prototype of Er laser and delivery system Alta PE-AT (Dental Photonics, Inc.).
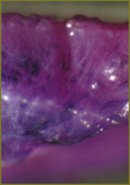
Results. We performed a microperforation of a 1 mm thick gingiva and created a microcrater (tunnel) in the underlying bone using a single pulse with energy 5, 10 and 30 mJ. The laser tunnel characteristics in the gingiva, bone and dentine were characterized as a function of laser irradiation parameters. Optical microscopy and histology examination did not reveal carbonization or significant collateral damage of the bone tissue.
Conclusion. Using a laboratory prototype of Alta PE-AT Er laser we demonstrated feasibility of through gingiva laser microperforation of alveolar bone that can serve as the first step towards further study of healing and initiation of the alveolar bone regeneration.
- Ishikawa I., Sculean A. Laser dentistry in periodontics. In: Gutknecht N., editor. 1st International workshop of evidence based dentistry on lasers in dentistry. Quintessence Publishing 2007; 115–129.
- Kreisler M., Al Haj H., d’Hoedt B. Clinical efficacy of semiconductor laser application as an adjunct to conventional scaling and root planing. Lasers Surg Med 2005 Dec; 37(5): 350–355.
- Coleton S. Lasers in surgical periodontics and oral medicine. Dent Clin North Am 2004 Oct; 48(4): 937–962, vii.
- Schwarz F., Aoki A., Becker J., Sculean A. Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 2008 Sep; 35(8 Suppl): 29–44.
- Manni J.G. Dental applications of advanced lasers (DAAL). JGM Associates, Inc.; 2007.
- Belikov A.V., Erofeev A.V., Shumilin V.V., Tkachuk A.M. Comparative study of the 3 μm laser action on different hard tooth tissue samples using free running pulsed Er-doped YAG, YSGG, YAP and YLF lasers. Dental Applications of Lasers 1993; SPIE 2080: 60–77.
- Aoki A., Mizutani K., Takasaki A.A., Sasaki K.M., Nagai S., Schwarz F., et al. Current status of clinical laser applications in periodontal therapy. Gen Dent 2008 Nov–Dec; 56(7): 674–687; quiz 688–689, 767.
- Cobb C.M., Low S.B., Coluzzi D.J. Lasers and the treatment of chronic periodontitis. Dent Clin North Am 2010 Jan; 54(1): 35–53.
- Cobb C.M. Lasers in periodontics: a review of the literature. J Periodontol 2006 Apr; 77(4): 545–564.
- Sculean A., Chiantella G.C., Arweiler N.B., Becker J., Schwarz F., Stavropoulos A. Five-year clinical and histologic results following treatment of human intrabony defects with an enamel matrix derivative combined with a natural bone mineral. Int J Periodontics Restorative Dent 2008 Apr; 28(2): 153–61.
- Gaspirc B., Skaleric U. Clinical evaluation of periodontal surgical treatment with an Er:YAG laser: 5-year results. Journal of Periodontology 2007 Oct; 78(10): 1864–1871.
- Crespi R., Cappare P., Toscanelli I., Gherlone E., Romanos G.E. Effects of Er:YAG laser compared to ultrasonic scaler in periodontal treatment: a 2-year follow-up split-mouth clinical study. J Periodonto 2007 Jul; 78(7): 1195–1200.
- Yoshino T., Aoki A. Oda S., Takasaki A.A., Mizutani K., Sasaki K.M., et al. Long-term histologic analysis of bone tissue alteration and healing following Er:YAG laser irradiation compared to electrosurgery. Journal of Periodontology 2009; 80(1): 82.
- Pourzarandian A., Watanabe H., Aoki A., Ichinose S., Sasaki K.M., Nitta H., et al. Histological and TEM examination of early stages of bone healing after Er:YAG laser irradiation. Photomed Laser Surg 2004 Aug; 22(4): 342–350.
- Hibst R. Lasers for caries removal and cavity preparation: State of the art and future directions. J Oral Laser Appl 2002; 2: 203–211.
- Needleman I.G., Worthington H.V., Giedrys-Leeper E., Tucker R.J. Guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst Rev 2006(2): CD001724.
- Lukinykh L., Zhulev E., Chuprunova I. Bolezni parodonta. Klinika, diagnostika, lechenie i profilaktika [Periodontal diseases. Clinical picture, diagnosis, treatment and prevention]. Nizhny Novgorod: Izdatel’stvo Nizhegorodskoy gosudarstvennoy meditsinskoy akademii 2005; 322 p.
- Verdugo F., D’addona A. Long-term stable periodontal regeneration by means of autologous bone grafting in patients with severe periodontitis. Int J Periodontics Restorative Dent 2012 Apr; 32(2): 157–164.
- Needleman I., Tucker R., Giedrys-Leeper E., Worthington H. A systematic review of guided tissue regeneration for periodontal infrabony defects. J Periodontal Res 2002 Oct; 37(5): 380–388.
- Pinheiro A.L., Martinez Gerbi M.E., de Assis Limeira F. Jr., Carneiro Ponzi E.A., Marques A.M., Carvalho C.M., et al. Bone repair following bone grafting hydroxyapatite guided bone regeneration and infra-red laser photobiomodulation: a histological study in a rodent model. Lasers Med Sci 2009 Mar; 24(2): 234–240.
- Gladkova N.D., Karabut М.М., Kiseleva Е.B., Fomina Y.V., Muraev А.А., Balalaeva I.V., Feldstein F.I. Prizhiznennyy kontrol’ regeneratsii slizistoy obolochki polosti rta posle fraktsionnogo lazernogo fototermoliza metodom krosspolyarizatsionnoy opticheskoy kogerentnoy tomografii [Life-time control of oral mucosa regeneration after fractional laser photothermolysis using cross-polarization optic coherence tomography]. Sovrem Tekhnol Med — Modern Technologies in Medicine 2012; 2: 13–19.
- Romanos G.E., Gladkova N.D., Feldchtein F.I., Karabut M.M., Kiseleva E.B., Snopova L.B., et al. Oral mucosa response to laser patterned microcoagulation (LPM) treatment. An animal study. Lasers Med Sci 2013 Jan; 28(1): 25–31.
- Hantash B.M., Bedi V.P., Kapadia B., Rahman Z., Jiang K., Tanner H., et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 2007 Feb; 39(2): 96–107.
- Korzh N.A., Dedukh N.V. Reparativnaya regeneratsiya kosti: sovremennyy vzglyad na problemu. Stadii regeneratsii [Reparative bone regeneration: current view of the problem. Regeneration stages]. Ortopediya, travmatologiya i protezirovanie — Orthopedics, traumatology and prosthetic repair 2006; 1: 77–84.
- Mayborodin I.V., Drovosekov M.N., Toder M.S., Matveeva V.A., Kolesnikov I.S., Shevela A.I. Regeneratsiya povrezhdennoy kosti nizhney chelyusti krys na fone vvedeniya autologichnykh mezenkhimal’nykh stvolovykh kletok kostnomozgovogo proiskhozhdeniya [Regeneration of rat damaged mandibular bone against the background of introduction of autologous mesenchymal stem marrow cells]. Fundamental’nye issledovaniya — Fundamental Researches 2011; 9: 264–269.
- Mcdavid V.G., Cobb C.M., Rapley J.W., Glaros A.G., Spencer P. Laser irradiation of bone: III. Long-term healing following treatment by CO2 and Nd:YAG lasers. J Periodontol 2001 Feb; 72(2): 174–82.
- Friesen L.R., Cobb C.M., Rapley J.W., Forgas-Brockman L., Spencer P. Laser irradiation of bone: II. Healing response following treatment by CO2 and Nd:Yag lasers. J Periodontol 1999 Jan; 70(1): 75–83.
- Wang X., Zhang C., Matsumoto K. In vivo study of the healing processes that occur in the jaws of rabbits following perforation by an Er,Cr:YSGG laser. Lasers Med Sci 2005; 20(1): 21–27.
- Queiroga A., Sousa F., Araújo J., Santos S., Sousa C.F., Quintans T., et al. Evaluation of bone repair in the femur of rats submitted to laser therapy in different wavelengths: an image segmentation method of analysis. Laser Physics 2008; 18(9): 1087–1091.










