Ximedon Administration in Complex Treatment of Chemical Burns of Esophagus and Stomach in Experiment
The aim of the investigation was to study in experiment the morphological changes in rat esophageal and gastric tissues after chemical burn using a regeneration enhancing agent (Ximedon) against the background of medical treatment.
Materials and Methods. Esophageal and gastric chemical burns were modeled on Wistar white rats (n=70) by 30% acetic acid. The survivors were divided into three groups: a control group (without therapy), a standard treatment group (the rats were administered cefotaxime and prednisolone intraperitoneally) and an experimental group (cefotaxime, prednisolone, Ximedon intraperitoneally). The results were assessed morphologically and morphometrically on day 13, 19 and 40.
Conclusion. Esophageal and gastric mucosa thickness after chemical burn does not recover under any treatment. Antibiotics and corticosteroids taken after burn inhibit inflammation in tissues, but do not prevent scar tissue development in muscularis mucosae. A long term (6 weeks) of Ximedon therapy along with standard therapy results in complete recovery of esophageal and gastric mucous structure and significantly suppresses a scarring process in muscular elements.
Studies devoted to chemical burns and cicatricial esophagostenoses are being actively continued and serve as a confirmation of difficulty of the problem and urgency of further studies.
According to American Association of Poison Control Centers only in 2008 more than 1.6 million cases of children poisoning occurred and alkaline esophageal burns were recorded in 18–46% cases after the use of various consumer chemicals [1].
Analyzing the treatment of esophagitis after burn in children referred to the Abbass Children Hospital (Iran) within the period 2009–2011 a group of authors [2] shows the predominance of city population in the structure of admitted patients and assesses the incidence of this abnormality to be 15.8 per 10 000. Moreover, comparing the results of their studies with those of American, Turkish and Egyptian hospitals Sakineh Fallahi et al. indicate a higher percentage of severe patients in developing countries.
In Russia the patients with acute chemical upper gastrointestinal injuries amount to 10–32% of all admitted to acute poisoning treatment centers [3], and the use of acetic acid ranks first in the structure of damaging agents (up to 40%) [4].
The complications of chemical burns of upper digestive tract are development of scarring esophageal and gastric strictures, early and late bleedings, esophageal perforations. The nervous system, lungs, liver and kidney are jeopardized, and in some cases it may result in lethal income [2].
According to the data of the professional medical association [5], esophageal stenosis occurs in 5% cases. The same source shows the risk of esophageal squamous cell cancer in patients with esophageal stenoses after burn to increase by 1000 times.
Modern approach of treatment of severe chemical esophageal and gastric burns along with the measures aimed at correction of impairments of the whole body includes antimicrobial therapy, the use of corticosteroids, prevention of gastroesophageal reflux, different methods of adaptation [5–7] and occasionally — surgical treatment [8].
Current clinical studies prove the effectiveness of a short-term course of corticosteroids [5, 7].
Physiotherapeutic procedures (local diathermia, darsonvalization, intra-esophageal electrophoresis), hyperbaric oxygenation, intra-esophageal laser therapy are currently proposed as the measures enhancing regeneration [3].
Data on the use of medications enhancing regeneration in the treatment of chemical esophageal and gastric lesions are virtually missing. In this group of drugs Ximedon arouses special interest, and according to the experimental and clinical data it significantly exceeds alternative drugs by its effect. In addition, it has high anabolic and anticatabolic activity, stimulates erythro- and leucopoiesis, cellular and humoral protective factors, and has an anti-inflammatory and antimicrobial effect [9].
The aim of the investigation was to study in experiment morphological changes in rat esophageal and gastric tissue after chemical burn using a regeneration enhancing agent (Ximedon) against the background of standard medical treatment.
Material and Methods. On the basis of the Central Research Laboratory of the Nizhny Novgorod State Medical Academy (Russia) chemical esophageal and gastric burn was simulated in experiments on rats. The work was performed in full conformity with the ethical principles according to European Convention for the protection of vertebrata used for experimental and other scientific purposes (the Convention was passed in Strasburg, 18.03.1986, and adopted in Strasburg, 15.06.2006).
70 Wistar white rats, weighting 200–250 g, were enrolled in the experiment. The animals were divided into three groups and marked. The anesthetized rats were anesthetized by 30% acetic acid. 19 animals died for the first three days. Moreover, macro- and microscopic signs of esophageal and gastric burn were found in experimental rats on day 5 only. A control group (group 1) (n=12) throughout the experiment was given usual food and had standard water schedule without treatment. Group 2 (n=15) on day 5 after inoculation began to receive the standard treatment: antimicrobial cefotaxime — 100 mg/kg, 7 days, prednisolone — 1 mg/kg, for 3 days. Both medications were given intraperitoneally once a day. In experimental group (group 3) (n=24) beginning from day 5 the treatment with cefatoxime and prednisolone was combined with intraperitoneal administration of 3% Ximedon solution 30 mg/kg once a day. The animals of this group were divided into two subgroups. In subgroup 3a (n=15) the animals were administered a short-term course of Ximedon (7 days) and in subgroup 3b (n=9) Ximedon was given throughout the experiment. The animals of groups 2 and 3 also had their usual food and water schedule. Rats in all groups were sacrificed by decapitation on day 13, 19 and 40. The fragments of esophagus, stomach were taken from the animals for morphological investigation. The material was fixed in 10% solution of neutral formalin, embedded in paraffin followed by the preparation of paraffin blocks. Slices were prepared in compliance with anatomical orientation and stained with hematoxilin-eosin and by van Gieson. The prepared samples were studied light-optically (Leica DM 1000, Germany) with photo-fixation of an image (Leica DFC290, Germany). For comparable assessment of results morphometry was applied using ocular micrometer. The thickness of all mucous membranes and appropriate parts of esophageal and gastric muscle plate was measured in standard units.
In statistical data processing for comparable samplings having normal distribution Student t-test was used. If however any of the compared samplings had no normal distribution, Mann–Whitney test was applied. P=0.05 was considered significant difference.
Results and Discussion. In the samples obtained from all rats on day 5 (before treatment start) in the wall of lower esophagus and stomach nectrotic processes predominated in some cases extending on the submucous layer and muscular layer, and there was also lympho-leukocyte infiltration in submucous layer and muscular layer (Fig. 1). Most severe changes were localized in the region of esophagogastric junction and on the boundary of glandular and aglandular gastric area.
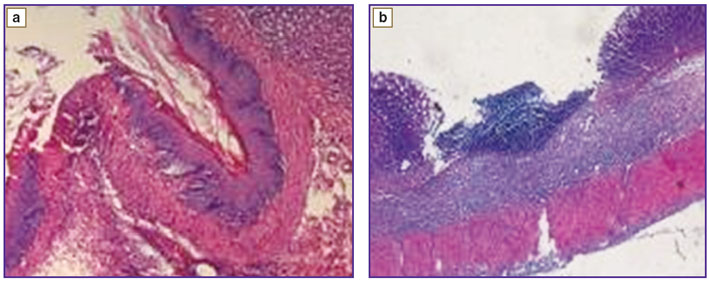 Fig. 1. Chemical burn in 5 days (before treatment): a — esophageal ulcer, ×100; b — gastric ulcer, ×40. Hematoxilin-eosin staining Fig. 1. Chemical burn in 5 days (before treatment): a — esophageal ulcer, ×100; b — gastric ulcer, ×40. Hematoxilin-eosin staining
|
On day 13 in the samples of control group edema of submucous layer, dense neutrophil infiltration up to muscular layer were found. In groups 2 and 3 on day 13 macro- and microscopic inflammatory changes were less severe but in the experimental group enhanced regeneration of esophageal and gastric mucous membrane was also found in the form of increased number of basal layer cells.
In the samples obtained on day 19 in the control group inflammation signs remained in the form of diffuse lymphocytic infiltration, along with pronounced regeneration of the mucous membrane signs of muscle plate fibrosis. In group 2 samples (with standard treatment) and subgroup 3a (a short-term course of Ximedon) inflammation signs also remained, however leukocytic infiltration was observed in the form of lesions, and presented by lymphocytes and eosinophils, edema of submucous layer being notable. Fibrosis signs were also present. In subgroup 3a compared with control and standard one infiltrative changes were significantly less severe, the structure of mucous membrane completely recovered. In subgroup 3b (a long-term course of Ximedon) the picture was similar to that in subgroup 3a but fibrosis signs were missing, hyperactivity of basal layer was found. Therefore, further study in the experimental group was performed using a long-term course of Ximedon.
On day 40 in treated rats of groups 2 and 3 compared with the control one macroscopically hyperemia of esophageal and gastric mucosa was less severe, there were no signs of secondary complications in animals (in a group without treatment multiple pulmonary abscesses were found in 1 rat). The sings of severe fibrosis of submucous layer were revealed in control samples (Fig. 2, a, 3, a). Collagen fibers grow between smooth muscle cells of muscularis mucosae whereby its fragmentation is noted. Mucosa thickens due to fibrosis. Submucous layer has moderate edema with vascular congestion. Solitary gastric erosions, remaining focal lymphocytic infiltration are found.
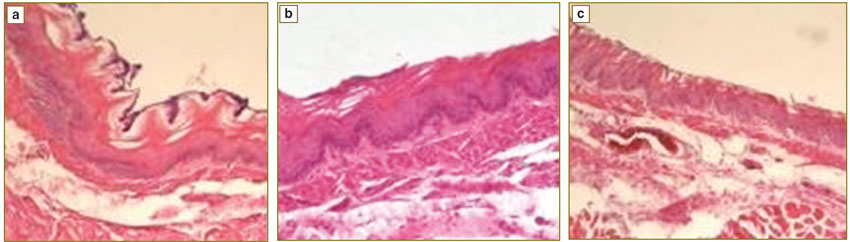 Fig. 2. Chemical burn of esophagus (day 40): a — control group; b — standard treatment; c — experimental group (with a long-term use of Ximedon). Hematoxilin-eosin staining. ×100 Fig. 2. Chemical burn of esophagus (day 40): a — control group; b — standard treatment; c — experimental group (with a long-term use of Ximedon). Hematoxilin-eosin staining. ×100
|
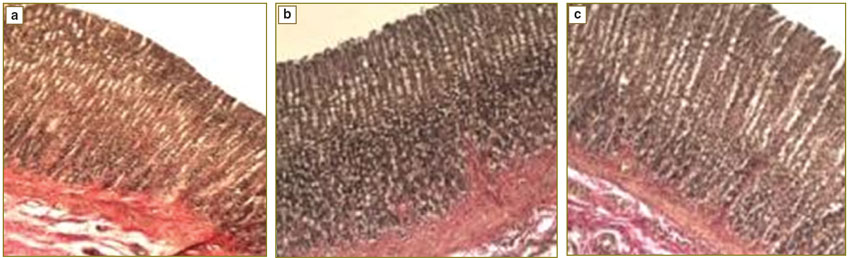 Fig. 3. Chemical burn of stomach (day 40): a — control group; b — standard treatment; c — experimental group (with a long-term course of Ximedon). van Gieson’s staining. ×100 Fig. 3. Chemical burn of stomach (day 40): a — control group; b — standard treatment; c — experimental group (with a long-term course of Ximedon). van Gieson’s staining. ×100
|
In a group with standard treatment microscopically changes are less marked and presented with edema of submucous layer, vascular congestion, eosinophil infiltration of proper mucous plate and submucous layer. Fibrosis signs of proper mucous plate were revealed (Fig. 2, b, 3, b). In the experimental group (in the subgroup with a long-term Ximedon administration) mucosa virtually recovered, there being no fibrosis of submucous layer (Fig. 2, c, 3, c).
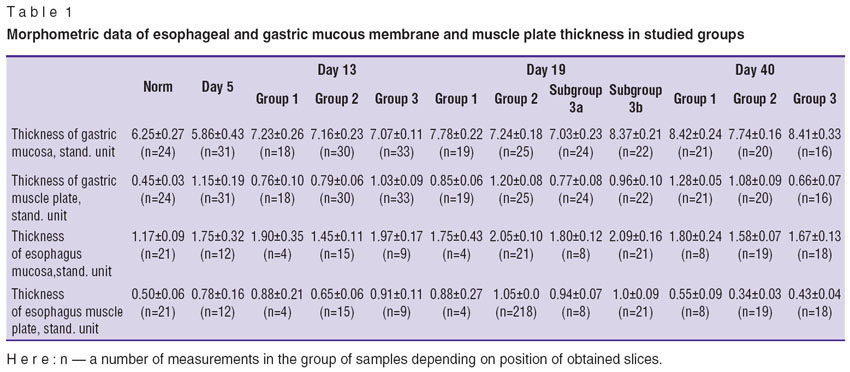
Morphometric data obtained in investigation of esophageal and gastric mucosa and muscle plate in all studied groups were compared with the known norm (Table 1). Esophageal and gastric mucosa thickness in all studied samples differed from normal one (Table 2).
|
Table 1. Morphometric data of esophageal and gastric mucous membrane and muscle plate thickness in studied group |
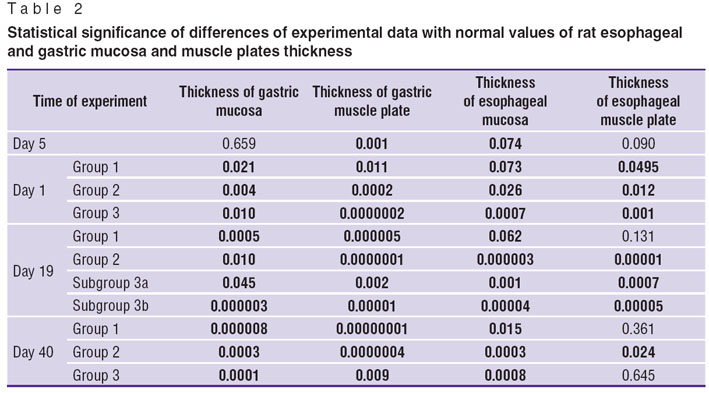 Table 2. Statistical significance of differences of experimental data with normal values of rat esophageal and gastric mucosa and muscle plates thickness Table 2. Statistical significance of differences of experimental data with normal values of rat esophageal and gastric mucosa and muscle plates thickness
|
Thus, esophageal and gastric mucosa thickness after chemical injury does not recover completely under a usual course or after any treatment.
Considering the importance of thickness assessment of muscle elements as the main characteristics participating in formation of stenoses after burn we analyzed the changes of esophageal and gastric muscle plates in studied groups over time (Fig. 4). The thickness increase of corresponding layer is consistent with the increase of edema at early stages along with edema sclerotic changes are found in tissues in later periods.
In the group with Ximedon (a long-term course of Ximedon) administration, smooth increase of esophageal muscle plate thickness is found at early stages due to edema progression and similar decrease by day 40 versus spasmodic changes in other groups (due to increase of sclerotic processes in tissue).
Most representative results were obtained in gastric samples (Fig. 4, b): gradual decrease of muscle plate was observed in an experimental group: morphometric values by day 40 were the most near-normal.
Thus, antimicrobial therapy and the use of corticosteroids in the treatment of chemical esophageal and gastric burns are justified since they contribute to inflammation reduction in impaired tissues. However, medicinal treatment does not prevent from developing scarring changes in the muscle plate of esophagus and stomach in case of chemical injury. A long-term administration of Ximedon (6 weeks) along with standard treatment regimen results in complete recovery of esophageal and gastric mucosa structure and suppresses a scarring process in musclular elements of mucosa. However, in a standard course of the disease and under different treatment no complete recovery of esophageal and gastric mucosa thickness occurs, it requiring a long-term follow up after chemical burns of stomach and esophagus.
Conclusion. Esophageal and gastric mucosa thickness after chemical burn does not recover under any treatment. Antimicrobials and corticosteroids taken after chemical burn inhibit inflammation in tissues, but do not prevent scar tissue development in muscularis mucosae. A long-term course (6 weeks) of Ximedon therapy along with standard therapy results in complete recovery of esophageal and gastric mucosa structure and significantly suppresses a scarring process in musclular elements.
Study Funding and Conflict of Interests. The study was not supported by any funds, and the authors have no conflict of interest to disclose.
References
- George D. Ferry, Douglas S. Fishman. Caustic esophageal injury in children. 2013.www.uptodate.com/contents/caustic-esophageal-injury-in-children.
- Sakineh Fallahi, Seyed M.V. Hosseini, Soghra Fallahi, Morteza Salimi, Ali Akbar Hesam, Seydeh Hamideh Hoseini. Extent of injury of gastrointestinal tract due to accidental ingestion of chemicals among children at Bandar Abbass Children Hospital 2009–2011. Life Science Journal 2012; 9(4): 2054–2058.
- Volkov S.V., Ermolov A.S., Luzhnikov E.A. Khimicheskie ozhogi pishchevoda i zheludka (endoskopicheskaya diagnostika i lazeroterapiya) [Chemical burns of esophagus and stomach (endoscopic diagnosis and laser therapy)]. Moscow: Izdatel’skiy dom “Medpraktika-M”; 2005; 120 p.
- Rukevich S.G., Parshikov V.V., Batanov G.B., Karpova I.Yu. Primenenie sovremennoy klassifikatsii mnogokomponentnykh prizhigayushchikh veshchestv pri khimicheskikh ozhogakh pishchevoda i zheludka u detey. V kn.: Sbornik nauchnykh rabot konferentsii, posvyashchennoy 100-letiyu so dnya rozhdeniya professora A.A. Dikovoy [Application of modern classification of multicomponent cauterants in chemical burns of esophagus and stomach in children. In: Collection of scientific papers of the conference devoted to the 100th anniversary of the birth of Prof. A.A. Dikova]. Nizhny Novgorod; 2013.
- Corrosive esophageal injury. Professional health care portal “Health writing”. 2007.http://www.health-writings.com/corrosive-esophageal-injury/.
- Razumovskiy A.Yu., Obydennova R.V., Kulikova N.V., Alkhasov A.B., Rachkov V.E., Mitupov Z.B., Masenkov Yu.I. Evolyutsiya vzglyadov na khirurgicheskoe lechenie detey s khimicheskimi ozhogami pishchevoda [The evolution of surgical treatment for children with chemical burns of the esophagus]. Rossiyskiy vestnik detskoy khirurgii, anesteziologii i reanimatologii — Russian Vestnik of Pediatric Surgery, Anesthesiology and Resuscitation 2011; 1: 51–59.
- Alekseenko S.I., Bairov V.G., Tsurikova G.P., et al. Khimicheskie ozhogi pishchevoda u detey. V kn.: Sovremennye tekhnologii diagnostiki i lecheniya detey i podrostkov. Vypusk 2 [Chemical burns of esophagus. In: Modern technologies in diagnosis and treatment of children and adolescents]. Issue 2. Saint Petersburg; 2005; р. 25–30.
- Makarova O.L., Korolev M.P., Fedotov L.E. Taktika lecheniya bol’nykh s sochetannymi rubtsovymi strikturami pishchevoda i zheludka posle khimicheskikh ozhogov [Management of patients with concomitant esophageal and gastric corrosive strictures after chemical burns]. Ukrainskiy zhurnal maloinvazivnoy i endoskopicheskoy khirurgii — Ukrainian Journal of Minimally Invasive and Endoscopic Surgery 2003; 7(3): 39–40.
- Izmaylov S.G., Izmaylov M.Yu., Aver’yanov M.Yu., Reznik V.S. Ksimedon v meditsinskoy praktike [Ximedon in medical practice]. Nizhny Novgorod: Izdatel’stvo Nizhegorodskoy gos. med. akademii; 2001; 188 p.










