Modern Capabilities of Surgical Management of Patients with Open-Angle Glaucoma Combined with Cataract
Cataract and glaucoma affecting mainly elderly people sometimes are associated; therefore the problem of their combined treatment is urgent.
The aim of the investigation was to assess the efficiency of modern surgery in patients with combined cataract and open-angle glaucoma.
Materials and Methods. The present open prospective study is based on the examination and surgery findings of patients with associated cataract and different stages of open-angle glaucoma (200 eyes). Depending on surgery type patients were divided into three groups. Group 1 included 81 patients (100 eyes) with combined cataract and glaucoma stabilized by medical treatment, who underwent phacoemulsification with intraocular lens implantation. Group 2 consisted of 44 patients (50 eyes) with cataract associated with open-angle glaucoma, who underwent phacoemulsification with intraocular lens implantation in combination with sinusotomy with viscocanalodilatation. 44 patients (50 eyes) with associated cataract and glaucoma, in whom phacotrabeculectomy was performed, composed group 3. Most patients had developed and advanced stages of glaucoma (81%). In addition, in the majority of patients the pseudoexfoliation syndrome (71.5%) was found.
Results. Phacotrabeculectomy and phacoemulsification with viscocanalodilatation were found to have a marked hypotensive effect in significant improvement of visual function in patients with associated cataract and glaucoma, regardless of glaucoma stage and pseudoexfoliation syndrome presence. Moreover, phacoemulsification with sinusotomy and viscocanalodilatation provides earlier visual acuity recovery with less early postoperative complications compared to phacotrabeculectomy, and hypotensive effect is comparable to phacotrabeculectomy after additional laser goniopuncture which was required postoperatively in 58% cases. Phacoemulsification, being a less traumatic procedure, causes less postoperative complications in patients with associated cataract and glaucoma, however, a hypotensive effect is sufficient only with additional medical therapy.
Cataract and glaucoma are diseases, which form the basis of ophthalmosurgical pathology worldwide. According to different authors, the prevalence of their association is 14–76% [1, 2]. Patients with glaucoma have an increased risk of cataract [3].
Since so called anti-glaucoma surgical procedures aim at intraocular pressure (IOP) lowering, over the years, ophthalmologists throughout the world were interested in choosing most effective IOP-lowering procedure in patients with associated glaucoma and cataract [4–7].
There are three main surgical approaches in treatment of patients with associated cataract and glaucoma:
two-step treatment — IOP-lowering surgical procedure as a first step, and cataract extraction as a second step; or phacoemulsification (PE) followed by IOP-lowering procedure;
cataract extraction alone;
combined procedure.
Two-step treatment is indicated if incipient cataract reduces vision only slightly, or in cases when an extraction of a cloudy lens is indicated, but there is a risk of serious complications due to steady high IOP. A broadening of indications for two-step treatment is not justified, since cataract extraction after IOP-lowering surgery can involve considerable difficulties. Moreover, a psychological aspect is of great importance: the waiting period before the second surgery reduces the quality of patient’s life and affects his attitude towards a successful ultimate result.
In recent years, under two-step treatment many ophthalmologists understand PE as the first step, and if required, IOP-lowering surgery — as the second step — due to the belief that PE itself is a hypotensive procedure [8–11].
In some cases, despite the presence of associated open-angle glaucoma (OAG), surgery may be limited only to PE with intraocular lens (IOL) implantation. This approach is useful if a patient has incipient OAG, no evident visual field and optic disc changes, and IOP is normalized by minimal therapy.
The following facts speak for combined surgeries: IOP reduction and cloudy lens extraction during the same surgical procedure, a faster rehabilitation period compared to two-step treatment. A small incision in combination with PE and IOP-lowering surgery is of outmost importance. The incision enables to maintain the anterior chamber depth during surgery minimizing the risk of expulsive hemorrhage, as well as provides quick visual recovery with stable postoperative refraction and only slight surgery-induced astigmatism.
Among basic combined surgical techniques, there is a combination of cataract extraction with IOP-lowering procedures of penetrating and non-penetrating types. Currently, cataract extraction is usually performed as PE, therefore a combined technique of PE and trabeculectomy was widely accepted, and in 1991 it was termed “phacotrabeculectomy” [12]. Filtration surgery has both advantages and disadvantages. Significant IOP decrease for many years can be referred to advantages. However, sudden intra-operative IOP drop could result in serious problems both during the surgery and postoperatively. There is an increased risk of hemorrhagic complications, ciliochoroidal detachment, shallow anterior chamber syndrome, severe postoperative hypotony, etc.
Non-penetrating surgery for the treatment of OAG patients has gained currency and became a wide-spread method. These procedures are performed without opening the eyeball, what significantly reduces both intraoperative and postoperative complication risk. IOP-lowering effect comparable with that of trabeculectomy is achieved by the procedure followed by laser goniopuncture.
Data presented here determine further investigation of the efficacy of some modern surgical techniques used in the treatment of patients with associated cataract and glaucoma.
The aim of the investigation was to assess the efficacy of modern surgery in patients with cataract associated with open-angle glaucoma.
Materials and Methods. The present open prospective study is based on the examination results and follow-up findings of patients with cataract associated with OAG (200 eyes). Mean age of patients was 72.20±0.57 years.
The study complies with the declaration of Helsinki (adopted in June, 1964 (Helsinki, Finland) and revised in October, 2000 (Edinburg, Scotland)), and was performed following approval by the local ethic committee of First Saint-Petersburg State Pavlov Medical University. Written informed consent was obtained from all patients.
Cataract maturity degree was assessed according to LOCS III (The lens opacities classification system III) [13].
Inclusion criteria were: age-related cataract associated with OAG; age ≥40 years; all surgeries were performed by the same surgeon.
Exclusion criteria were: earlier surgeries of the same eye; inflammatory diseases of the eye and his adnexa. In accordance with the research objectives all patients were divided into three groups according to surgery type (Table 1).
Table 1. Groups of patients/eyes according to surgery types 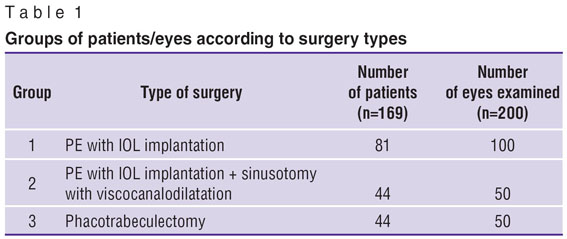
|
Group 1 included 81 patients with cataract associated with OAG in incipient, developed, and advanced stages and IOP stabilized by minimal treatment (Table 2). In group I patients, PE alone was performed. The group included 17 patients with advanced glaucoma in whom initial IOP at diagnosis did not exceed normal values on monotherapy or therapy with two IOP-lowering drugs. Patients were told about combined surgery option, but refused.
Table 2. Distribution of cases (eyes) in groups by glaucoma stages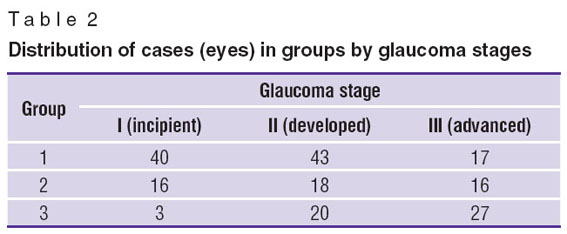
|
Group 2 included 44 patients (50 eyes) with cataract associated to OAG, who underwent PE combined with sinusotomy and viscocanalodilatation (IOP-lowering procedure of non-penetrating type). Group 3 consisted of 44 patients (50 eyes) with cataract associated to OAG, in whom phacotrabeculectomy alone was performed (IOP-lowering procedure of penetrating type).
Groups 2 and 3 were studied, aiming to:
1) reveal the advantages and disadvantages of PE with hypotensive procedures of penetrating and non-penetrating types;
2) decide in what cases non-penetrating procedures are preferable taking into consideration their unstable IOP-lowering effect and further need to take a decision upon the necessity of additional laser goniopuncture;
3) decide when trabeculectomy is reasonable to perform, since it has a higher risk of complications typical for penetrating procedures, but provides an immediate hypotensive effect.
Most patients were admitted with developed and advanced glaucoma stages (81%).
The study was carried out from November 2009 till June 2012.
In preoperative and postoperative periods, patients underwent examination including viso- and refractometry, biomicroscopy, Goldmann’s tonometry, static computerized perimetry, imaging of optical disc (HRT II, Heidelberg Engineering GmbH, Germany), optical coherence tomography (Stratus OCT 3000, Carl Zeiss Meditec Inc., USA).
Surgery results in patients of all groups were assessed the day after surgery, at one week after surgery, as well as at 1, 3, 6, 12 and more months after the procedure. Visual acuity and IOP changes were studied based on analysis of variance for dependent samples.
Findings were statistically analyzed using statistic package SPSS. Qualitative data were compared using Fischer assay. Changes of quantitative values were assessed by variance analysis for repeated measurements. P=0.05 (p<α) was considered as significant difference. Data were presented as percentage ratio, or mean values.
Results and Discussion. In group 1, mean IOP immediately before surgery was 15.4 mm Hg. After the procedure, it statistically significantly decreased (p=0.0006). A week after surgery, mean IOP value was 14.7 mm Hg, in one year — 13.9 mm Hg (Fig. 1, а). All patients continued glaucoma therapy.
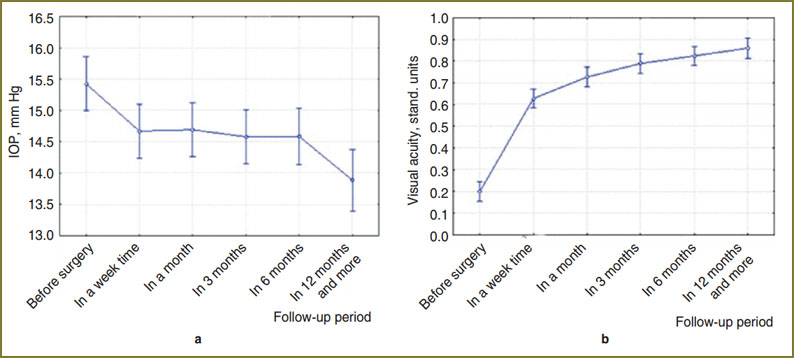 Fig. 1. Intraocular pressure (а) and visual acuity (b) dynamics after phacoemulsification Fig. 1. Intraocular pressure (а) and visual acuity (b) dynamics after phacoemulsification
|
In addition, in this group, there was a statistically significant increase in visual acuity (p<0.000001). Preoperative mean visual acuity was 0.2 (from 0.005 to 0.6). By postoperative days 3–5, mean value was up by 0.6 (from 0.005 to 1.0). Low vision during this period was revealed only in two patients, and was due to concomitant ophthalmic diseases. 0.005 visual acuity was found in a patient with marked epithelial and endothelial corneal dystrophy (later on, this patient’s visual acuity increased up to 0.3). Visual acuity of another patient with advanced glaucoma was 0.03 (his initial vision being 0.005). Visual acuity of other patients by days 3–5 after PE in no case was less than 0.1. In one year, mean visual acuity was 0.9 (Fig. 1, b).
Thus, patients with cataract associated with glaucoma stabilized by IOP-lowering therapy, who underwent PE with intraocular lens implantation with no combined antihypertensive procedure appeared to have statistically significant visual acuity increase and IOP reduction if instillation of hypertensive drugs was continued.
Findings after combined surgeries follow. Preoperative mean IOP in group 2 was 17.7 mm Hg, in group 3 — 18.5 mm Hg. These data do not mean that only patients with stabilized glaucoma and normal IOP values were operated. According to medical records, IOP values, as a rule, exceeded 30.0 mm Hg, and preoperative local and general antihypertensive therapy succeeded in reducing IOP immediately before the operation, aiming to minimize complications related to a sudden drop in pressure at eyeball opening. A week after surgery, IOP in group 2 reached 14.7 mm Hg, while in group 3 it was 11.2 mm Hg. After the first month post-op, IOP in patients after non-penetrating surgeries (15.0 mm Hg) also differed from that in patients after penetrating procedures (12.3 mm Hg) (Fig. 2, а).
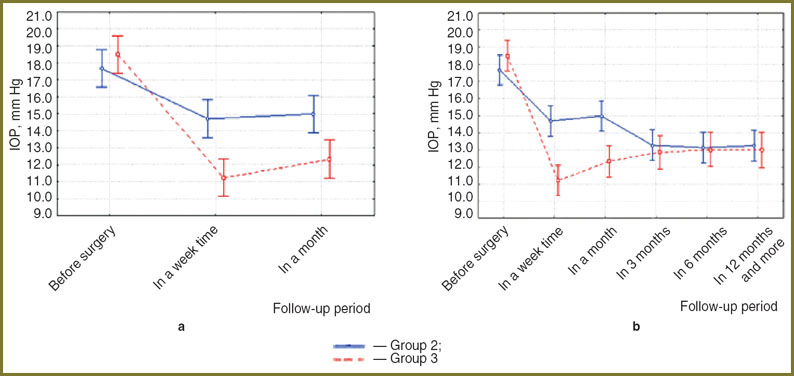 Fig. 2. Intraocular pressure dynamics according to surgery type: а — a month before laser goniopuncture in patients with PE combined with sinusotomy; b — throughout all the follow-up period Fig. 2. Intraocular pressure dynamics according to surgery type: а — a month before laser goniopuncture in patients with PE combined with sinusotomy; b — throughout all the follow-up period
|
The analysis of surgical results at 1 month after surgery showed 29 patients (58%) of group 2 to have IOP exceeding a target level, thus laser goniopuncture was required. After laser goniopuncture, IOP decreased.
Fig. 2, b demonstrates the curves of both groups to be almost the same by follow-up at month 3. IOP level after sinusotomy combined with PE decreased on average by 1.7 mm Hg amounting to 13.3 mm Hg, and almost reached mean IOP after phacotrabeculectomy (12.9 mm Hg).
A year after surgery, mean IOP in group 2 patients was 13.3 mm Hg, in group 3 patients — 13.0 mm Hg.
Thus, IOP dynamics before laser goniopuncture in patients after sinusotomy and viscocanalodilatation combined with PE significantly differed from that in patients with phacotrabeculectomy (p=0.00034).
Significant visual improvement was found in most patients of groups 2 and 3 (Fig. 3). However, vision changes after sinusotomy with viscocanalodilatation combined with PE significantly differed from those after phacotrabeculectomy (p=0.094).
Fig. 3. Dynamics of vision according to surgery type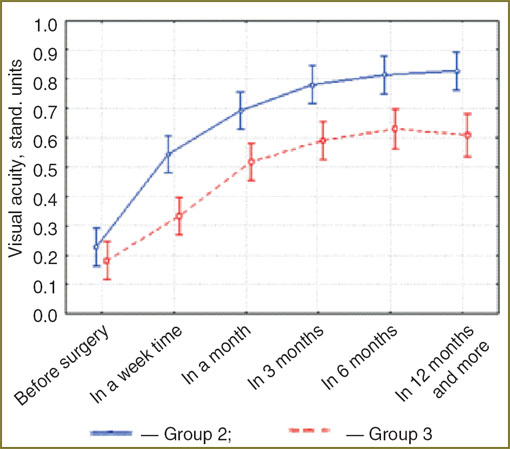
|
Mean preoperative visual acuity in patients of both groups was 0.2. A week after surgery, mean visual acuity of group 2 patients was 0.5, and of those in the third group — 0.3; and after one year and later — 0.8 in group 2, and 0.6 in group 3. Visual acuity increase was recorded in 100% of cases (50/50) in patients who underwent non-penetrating IOP-lowering surgery, and in 98% of cases (49/50) — in penetrating IOP-lowering procedures. Only one patient with advanced unstable glaucoma had unchanged visual acuity after phacotrabeculectomy — 0.005.
Since pseudoexfoliation syndrome (PEX) significantly impairs glaucoma process, in our study we recorded the presence or absence of pseudoexfoliation material deposition on corneal endothelium, along the pupil border, on the anterior lens surface, as well as in the iridocorneal angle area (Table 3). Further, particular emphasis was given to the assessment of surgical treatment efficacy in PEX patients.
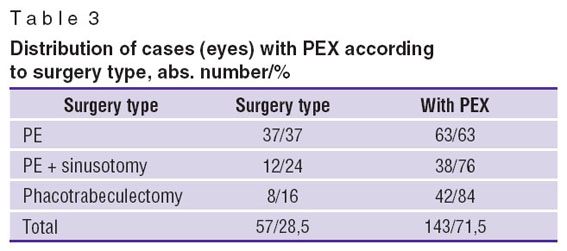 Table 3. Distribution of cases (eyes) with PEX according to surgery type, abs. number/% Table 3. Distribution of cases (eyes) with PEX according to surgery type, abs. number/%
|
Currently, one of the most important methods to diagnose and assess glaucoma stabilization is Heidelberg retina tomography (HRT) [14, 15]. At early postoperative period, HRT data remained unchanged in all patients included in the study. Later, insignificant negative dynamics was found in 5% out of 50 clinical observations after sinusotomy and viscocanalodilatation combined with PE, and in 12.5% out of 50 clinical observations in patients after phacotrabeculectomy.
During the study, visual field did not change in the overwhelming majority of patients. Slight positive dynamics was recorded in 18% patients (9/50) who underwent sinusotomy and PE, and in 14% of patients (7/50) after phacotrabeculectomy. Insignificant negative changes were found in 14% of cases (7/50) after a non-penetrating surgery, and in 4% of cases (2/50) after penetrating surgeries.
The analysis of the study results shows modern techniques used to treat patients with combined cataract and glaucoma to provide good IOP-lowering effect in both combined surgeries and in PE without “anti-glaucoma” component but using modern IOP-lowering drugs.
Conclusion. Phacotrabeculectomy and phacoemulsification with viscocanalodilatation achieve a marked IOP-lowering effect and result in significant improvement of visual function in patients with associated cataract and glaucoma, regardless of glaucoma stage and pseudoexfoliation syndrome presence.
Phacoemulsification with sinusotomy and viscocanalodilatation provides IOP-lowering effect comparable to that of phacotrabeculectomy after additional laser goniopuncture which was mandatory postoperatively in 58% of cases (29/50). Such surgical management provides earlier visual acuity recovery with less early postoperative complications compared to phacotrabeculectomy.
After phacoemulsification, patients with associated cataract and glaucoma are found to have less postoperative complications, however, the IOP-lowering effect is provided only if additional medical therapy is continued.
Study Funding and Conflict of Interests. The study was not supported by any funds, and the authors have no conflict of interest to disclose.
References
- Alekseev I.B., Mongush A.Kh. Kliniko-morfologicheskiy analiz ekstraktsii katarakty v kombinatsii s tsiklodializom ab interno. V kn.: Materialy VII s”ezda oftal’mologov Rossii [Clinicopathologic analysis of cataract extraction combined with cyclodialysis ab interno. In: Proceedings of VII Russian ophthalmology congress]. Moscow; 2000.
- Libman E.S., Chumaeva E.A. Epidemiologicheskie kharakteristiki glaukomy. V kn.: Glaukoma: teorii, tendentsii, tekhnologii. Sbornik statey IV Mezhdunarodnoy konferentsii [Glaucoma epidemiological characteristic. In: Glaucoma: theories, tendencies, technologies. Collected works of IV International conference]. Moscow; 2006; p. 203–213.
- Kass M.A., Heuer D.K., Higginbotham E.J., Johnson C.A., Keltner J.L., Miller J.P., Parrish R.K. 2nd, Wilson M.R., Gordon M.O. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002 Jun; 120(6): 701–713, http://dx.doi.org/10.1001/archopht.120.6.701.
- Astakhov S.Y. Sovremennye metody khirurgicheskoy reabilitatsii bol’nykh kataraktoy i glaukomoy. Dis. … dokt. med. nauk [Modern techniques of surgical rehabilitation of patients with cataract and glaucoma. Dissertation for the degree of Doctor of Medical Science]. Saint Petersburg; 1998.
- Aznabaev M.T., Alimbekova Z.F. Sovremennye podkhody k khirurgicheskomu lecheniyu katarakt pri pervichnoy otkrytougol’noy glaukome. V kn.: Materialy VII s”ezda oftal’mologov Rossii [Modern approaches to surgical management of primary open-angle glaucoma. In: Proceedings of VII Russian ophthalmology congress]. Moscow; 2000.
- Hudovernik M., Pahor D. Intraocular pressure after phacoemulsification with posterior chamber lens implantation in open-angle glaucoma. Klin Monbl Augenheilkd 2003 Dec; 220(12): 835–839, http://dx.doi.org/10.1055/s-2003-812552.
- Shingleton B.J. Heltzer J., O’Donoghue M.W. Outcomes of phacoemulsification in patients with and without pseudoexfoliation syndrome. J Cataract Refract Surg 2003 Jun; 29(6): 1080–1086, http://dx.doi.org/10.1016/S0886-3350(02)01993-4.
- Pohjalainen T., Vesti E., Uusitalo R.J., Laatikainen L. Phacoemulsification and intraocular lens implantation in eyes with open-angle glaucoma. Acta Ophthalmol Scand 2001 Jun; 79(3): 313–316, http://dx.doi.org/10.1034/j.1600-0420.2001.790322.x.
- Mathalone N., Hyams M., Neiman S., Buckman G., Hod Y., Geyer O. Long-term intraocular pressure control after clear corneal phacoemulsification in glaucoma patients. J Cataract Refract Surg 2005 Mar; 31(3): 479–483, http://dx.doi.org/10.1016/j.jcrs.2004.06.046.
- Mierzejewski A., Eliks I., Kaіuzny B., Zygulska M., Harasimowicz B., Kaіuzny J.J. Cataract phacoemulsification and intraocular pressure in glaucoma patients. Klin Oczna 2008; 110(1–3): 11–17.
- Augustinus C.J., Zeyen T. The effect of phacoemulsification and combined phaco/glaucoma procedures on the intraocular pressure in open-angle glaucoma. A review of the literature. Bull Soc Belge Ophtalmol 2012; (320): 51–66.
- Lyle W.A., Jin J.C. Comparison of a 3- and 6-mm incision in combined phacoemulsification and trabeculectomy. Am J Ophthalmol 1991 Feb 15; 111(2): 189–196.
- Chylack L.T. Jr., Wolfe J.K., Singer D.M., Leske M.C., Bullimore M.A., Bailey I.L., Friend J., McCarthy D., Wu S.Y. The lens opacities classification system III. The longitudinal study of cataract study group. Arch Ophthalmol 1993 Jun; 111(6): 831–836.
- Boland M.V., Quigley H.A. Evaluation of a combined index of optic nerve structure and function for glaucoma diagnosis. BMC Ophthalmol 2011 Feb 11; 11–16, http://dx.doi.org/doi:10.1186/1471-2415-11-6.
- Kilintzis V., Pappas T., Chouvarda I., Salonikiou A., Maglaveras N., Dimitrakos S., Topouzis F. Novel Heidelberg retina tomograph-based morphological parameters derived from optic disc cupping surface processing. Invest Ophthalmol Vis Sci 2011 Feb 16; 52(2): 947–951, http://dx.doi.org/10.1167/iovs.10-6298.










