The Evolution of the Local and System Therapy of Breast Cancer Stage I: 27-Years’s Data Analysis
The aim of the investigation is to study the dynamics of approaches in surgery, adjuvant radiotherapy and systemic therapy for breast cancer stage I over the past 27 years.
Materials and Methods. In the study included 1341 women (aged 21–88 years) with invasive breast cancer stage I, who had received treatment in N.N. Blokhin Russian Cancer Research Center and Clinic of RMAPE (Moscow) from 1985 to 2012. The first stage of treatment for all the patients included radical surgery (43.5% patients — radical mastectomy; and 56.5% — breast-conserving surgery). More than half of the patients (58.9%) received adjuvant radiotherapy; adjuvant systemic therapy was used in 821 patients (61.0%), endocrine therapy alone — in the third of patients (432 women, 32.1%), chemotherapy alone — in 124 women (9.2%), and 526 patients (19.7%) received a combined systemic therapy (chemotherapy and endocrine therapy). We analyzed the change of approach to the surgical treatment, adjuvant radiotherapy and systemic therapy from 1985 to 2012. A statistical analysis was made by international statistical program SPSS 20.0.
Results. Over the past 27 years local treatment structure of stage I breast cancer has changed: radiotherapy has become an indispensible part of breast conserving therapy, and was added by “boost” (radiotherapy with a dose of 14–16 Gy) on tumor bed by a half of women (50.3%). The part of patients who received radiotherapy after radical mastectomy has decreased (from 14.6 to 4.5%, p < 0.05). Adjuvant systemic therapy has been used by the majority of women (86.7%): a part of patients receiving endocrine therapy has significantly increased (from 20.7 to 44.3%), chemotherapy (from 2.6 to 13.6%), or chemo-hormone therapy (from 8.4 to 28.8%), p < 0.05. Chemotherapy regimens have been changed: non-anthracycline combinations are used instead of anthracycline regimens, and after 2005 — taxanes. HER2-status detection has been used in clinical practice since 2000, and trastuzumab in adjuvant therapy — after 2005; about half of the women with HER2-positive breast cancer stage I (50.8%) have received anti-HER2-therapy by trastuzumab. The proportion of patients receiving endocrine therapy by tamoxifen alone has decreased (from 84.2 to 52.4%, p < 0.05) in favor of other agents (aromatase inhibitors and sequential modes).
Breast cancer is the most common oncological pathology among female population worldwide, and its incidence rate is constantly growing [1, 2]. Many countries has introduced active mammography screening, it resulting in significant increase of early breast cancer (noninvasive and invasive breast cancer stage I) among newly diagnosed cases that has led to the change of paradigm of the treatment of this pathology [3, 4]. The decrease of primary tumor size has contributed to active introduction of breast conserving therapy, the necessity to prepare local treatment standards and radiotherapy reevaluation [5–8]. The study of biological characteristics of a tumor and its receptor status has resulted in the rise of drug therapy personalization and target therapy [9, 10]. The application of adjuvant systemic treatment is the most debating point in stage I breast cancer: even if there are such favorable prognostic factors as minimum size of a tumor and a negative regional lymph node status, true prognostic value of this therapy is still unstudied [11–13].
The aim of the investigation was to study the dynamics in approaches to local and systemic treatment of stage I breast cancer over the past 27 years, as well as the results of these changes.
Materials and Methods
Characteristics of patients and tumors. In the study included 1341 women with invasive breast cancer, T1a-b-cN0M0-stage, who had received their treatment in N.N. Blokhin Russian Cancer Research Center and Clinic of RMAPE (Moscow, Russia) from 1985 to 2012. The first stage of treatment for all the patients included radical mastectomy — 583 cases, 43.5%; 758 women (56.5%) underwent breast-conserving treatment; the patients’ age being 21–88 years, median — 52 years (Table 1).
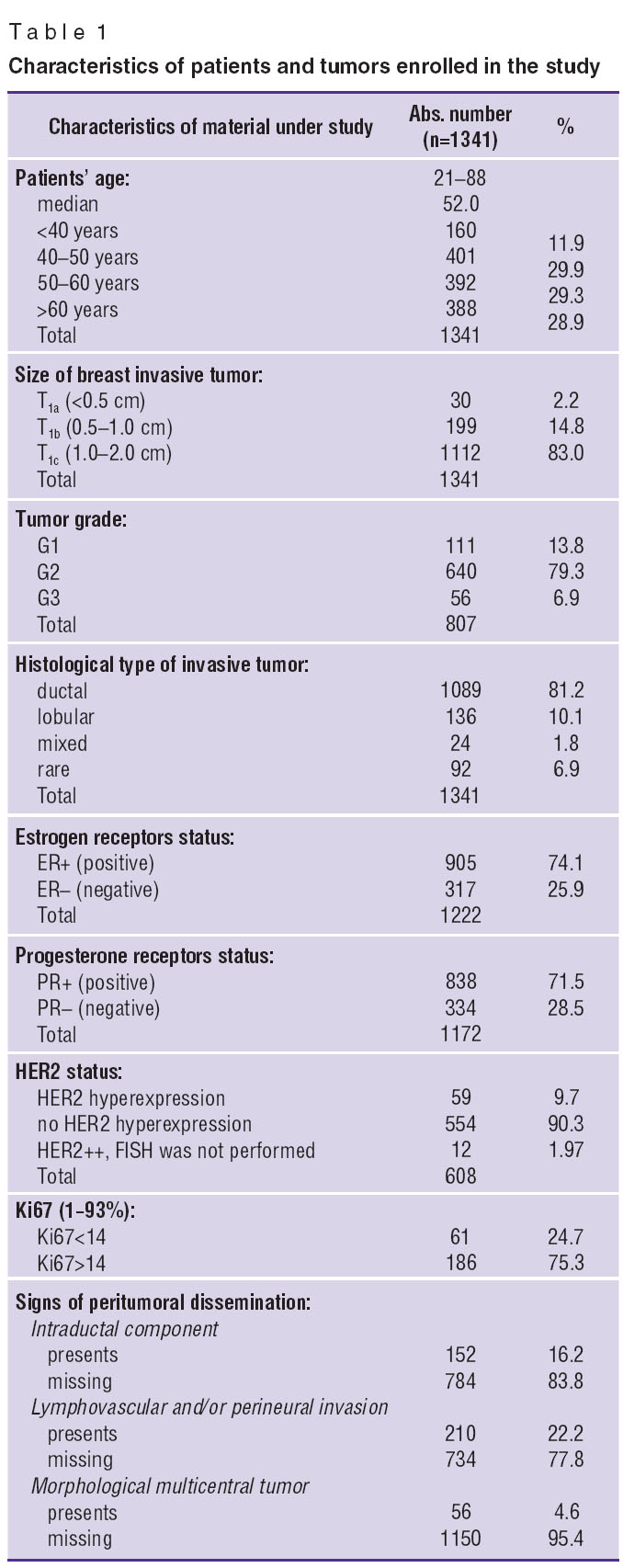 Table 1. Characteristics of patients and tumors enrolled in the study Table 1. Characteristics of patients and tumors enrolled in the study
|
This retrospective study was approved by the ethic committee of N.N. Blokhin Russian Cancer Research Center, Russian Academy of Medical Sciences and compliant with the Declaration of Helsinki (the Declaration was passed in Helsinki, Finland, June, 1964, and revised in October, 2000, Edinburg, Scotland). All patients admitted to N.N. Blokhin Russian Cancer Research Center and Clinic of RMAPE give the consent for their data to be used for scientific purposes.
According to routine morphological investigation of all patients (n=1341) the size of invasive tumor was up to 2.0 cm: micro-carcinomas — up to 0.5 cm (Т1а), n=30, 2.2%; tumors — 0.5–1.0 cm (Т1b), n=199, 14.8%; in most cases (n=1112, 83%) tumor size was 1.0–2.0 cm (Т1с). Anaplasia grade (G) was studied in 807 cases, moderately grade prevailed (G2) — 640/807 cases, 79.3%; high-differentiated tumors (G1) were found in 111/807 cases, 13.8%, and low-differentiated tumors (G3) — less frequently, in 56/807 cases (6.9%). Histological tumor variant was found in all women; there were prevailing infiltrative ductal carcinoma (1089 tumors, 81.2%), lobular carcinoma was revealed in 136 cases (10.1%), mixed cancer was rarely diagnosed (24 cases, 1.8%) (See Table 1). Tumors of rare infiltrative types (medullary, papillary, colloid, tubular, metaplastic and other) were found in 92 patients (6.9%). The status of estrogen receptors (ER) was studied in 1222 tumors, progesterone receptors (PR) — in 1172 cases; most patients had hormone-positive tumors: ER(+) — 905/1222 cases, 74.1%; PR(+) — 838/1172 cases, 71.6%. HER2-overexpression (HER2+++ in immunohistochemical (IHC) analysis; HER2++ and FISH- amplification positive) was revealed in 59 out of 608 examined tumors (9.7%). 550 tumors, 90.6%, were found to have no HER2-overexpression (HER0, HER1+ in IHC-analysis, as well as HER2++ and no FISH-amplification). It should be noted that in 12 patients IHC-analysis revealed HER2++ overexpression, however, FISH-reaction was not performed for some reasons; so, in this situation, HER2-status could not be interpreted as either positive or negative. Proliferative activity index Ki67 was assessed in IHC-analysis in 247 tumors and appeared to be from 1 to 93% (median — 24%). Most patients (186/247 cases, 75.3%) had tumors with high proliferative activity (Ki67>14%); tumors with low proliferative activity (Ki67<14%) were found in 61 out of 247 (24.7%). Multicentric tumors were revealed in 4.6% (56 out of 1206 tumors) cases in morphological investigation of urgical material. Intraductal component (dissemination of tumor cells along ducts beyond a primary tumor node) was found in 152 out of 936 cases (16.2%); the presence of lymphovascular and/or perineural invasion — in 210 out of 944 tumors (22.2%) (See Table 1).
Characteristics of the treatment provided and long-term results. More than half of the patients underwent adjuvant radiotherapy — 790/1341 cases, 58.9% (Table 2). Radiation of the remaining part of breast (± “boost” on bed of a removed tumor, where “boost” — radiotherapy at a dose of 14–16 Gy) is a necessary component of breast-conserving treatment; about half women in our study (675 out of 1341 cases, 50.3%) underwent breast-conserving surgery with radiotherapy. A part of women, who underwent radical mastectomy without radiotherapy, is also high — 468 out of 1341 (34.9%). Radiotherapy was rarely used after radical mastectomy (115 out of 1341, 8.6%) and included radiation exposure on postoperative scar, regional areas with or without parasternal lymph collector involved. Most frequently, the reasons for radiotherapy absence after breast-conserving surgery (83 out of 1341 cases, 6.2%) were a woman’s refusal or the presence of a serious pulmonary or cardiovascular comorbidity.
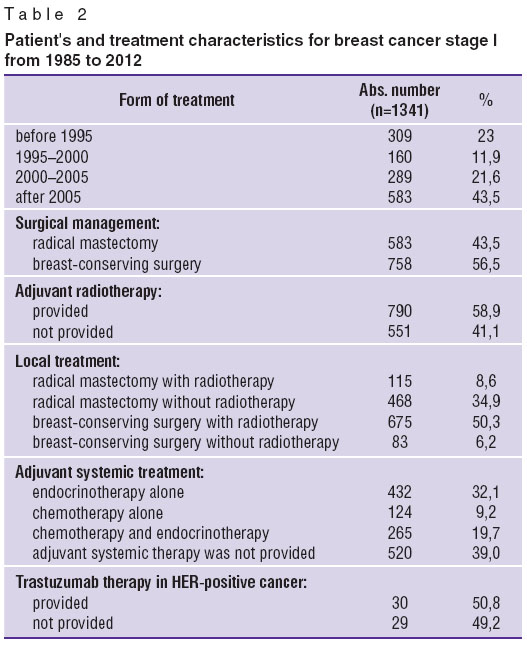 Table 2. Patient's and treatment characteristics for breast cancer stage I from 1985 to 2012 Table 2. Patient's and treatment characteristics for breast cancer stage I from 1985 to 2012
|
Adjuvant systemic therapy was administered to 821 out of 1341 women (61.0%); endocrinotherapy alone was used in a third of patients (432/1341 cases, 32.2%), chemotherapy alone — in 124/1341 (9.2%), and 526/1341 patients (19.7%) received combined systemic treatment (chemotherapy and hormonal treatment) (See Table 2). The analysis of chemotherapy regimens (we had the data on chemotherapy regimens used in 388 patients) showed the predominance of anthracycline-containing regimens (АС, САF, FEC and others) — 325 out of 388 cases (83.8%); 13 out of 388 (3.4%) patients received adjuvant chemotherapy with taxanes (paclitaxel or docetaxel) included; 12 out of 388 (3.1%) received combined (taxanes and anthracycline) chemotherapy regimens (simultaneous or sequential); other treatment schedules (anthracycline-free regimen — CMF, etc) were used in 38 out of 388 cases (9.8%). More than half of the patients with HER2-positive cancer (30 out of 59 women, 50.8%) were administered trastuzumab adjuvant therapy. The analysis of adjuvant hormonal treatment (data on hormonal treatment regimens of 694 patients were available) showed most women (427 out of 694; 61.5%) to be administered anti-estrogens only (tamoxifen, and others); aromatase inhibitors (anastrozole or letrozole) alone were administered to 100 out of 694 patients (14.4%); 16 out of 694 patients (2.3%) underwent castration alone; tamoxifen after castration was administered to 95 out of 694 women (13.7%), after castration aromatase inhibitors were taken less frequently (only in 5 cases, 0.7%); sequential administration of tamoxifen and aromatase inhibitors (2+3 or 3+2 years) was used in 51 out of 694 cases (7.4%).
A follow-up period was 6–312 months, median — 75 months. There are indices of total, recurrence-free and cancerspecific survival rate only for women followed up for at least 36 months — respectively, indices of 1209, 1167 and 1182 patients.
Recurrences were revealed in 255 out of 1167 followed up patients (21.9%); among them local recurrences amounting to 32.5% (83/255 cases), regional recurrences — 6.7% (17/255 cases) and distant metastases — 60.8% (155/255 cases). Time period before disease progression was 6–204 months, median — 36 months. During a follow-up 197 out of 1209 women (16.3%) died; in most cases (169 out of 197 patients, 85.8%) death was caused by cancer progression, and in 28/197 cases (14.2%) — by other causes.
In accordance with a period of primary tumor surgery, we divided the patients into four temporary groups: 1) group of patients treated before 1995 (309 women, 23.0%); 2) group of patients who underwent surgery in 1995–2000 — 160 women, 11.9%; 3) 289 women underwent treatment in 2000–2005, 21.6%, and 4) women who underwent surgery after 2005 — 583 women, 43.5%.
Local and systemic therapy changes over 25 years were studied in each group.
Statistic analyses was made by international statistical program SPSS 20.0. P-values of <0.05 were considered significant.
Results and Discussion. The comparison of surgical treatment characteristics in different time revealed no significant differences between groups in the volume of the performed operations: percentage of radical mastectomy before 1995 and after 2005 was identical (42.1 and 41.7%; p>0.05), from 1995 to 2000 there was a slight increase of preserving surgery up to 61.9%, with further decreasing up to 48.4% (from 2000 till 2005) that may be explained by a well-proven surgical technique and grouping of patients — possible candidates for breast-conserving surgery. Percentage of patients with adjuvant radiotherapy has changed slightly over the past 25 years (60.8% before 1995, and 59.7% after 2005; p>0.05). However, the comparison of local treatment showed significant differences (p<0.05): the number of patients who received adjuvant radiotherapy after radical mastectomy has decreased (14.6% before 1995, and 4.5% after 2005); breast-conserving surgery with radiotherapy has become a required standard resulting in significant decrease of patients, who used breast-conserving treatment without radiotherapy (11.7% before 1995, and 3.1% — after 2005). Therefore, most of women included in the study after 2005 underwent either radical mastectomy without radiotherapy (37.2%), or breast-conserving surgery with radiotherapy (55.2%).
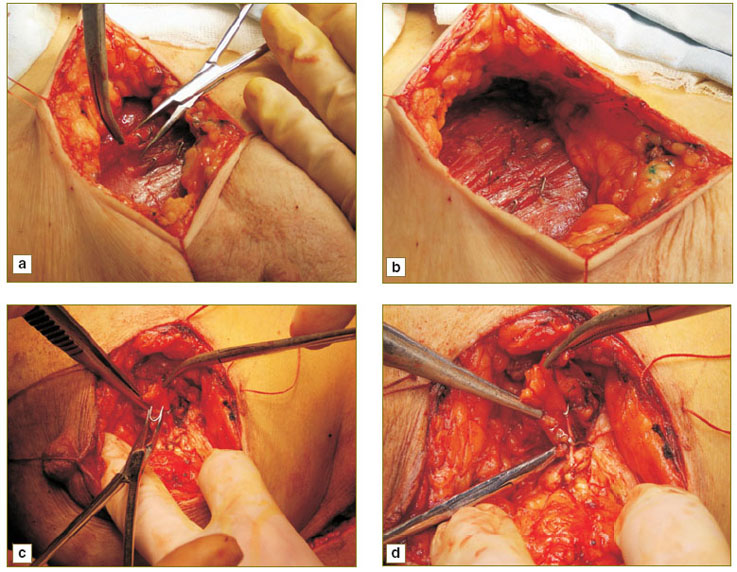
Moreover, about half of the patients, who had received conserving therapy after 2005 (155 out of 308, 50.3%), were administered external-beam therapy on the remaining breast part with secondary radiation of tumor bed at a dose of 10–16 Gy (“boost”). In accordance with international recommendations, “boost” was aimed at local control improvement in patients under 50 (in patients over 50 — only in case of high recurrence risk). Seromas, anatomical landmarks on CT-scans (Fig. 1), used to be the markings to determine a removed tumor bed when planning radiotherapy and it caused difficulties due to seroma resolution in course of time.
Fig. 1. Postoperative seroma on CT-scan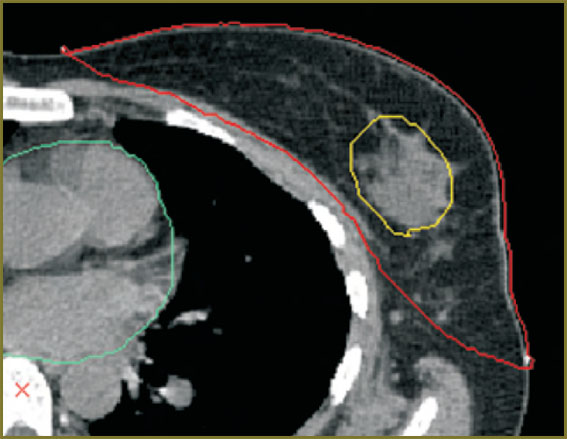
|
Since 2010, radiation field size, and depth of tumor bed have been determined using radiopaque clips made from titanium wire of a certain cross section, and applied by surgeons during the operation (Fig. 2). Titanium used for surgical clip production is biologically inert, radiopaque and nonmagnetic material.
The most significant changes were found when comparing adjuvant medical treatment modalities provided in different time periods (p<0.05). So, a proportion of patients who received adjuvant endocrinotherapy alone has increased from 20.7% (before 1995) to 44.3% (after 2005); and the number of women who recieved chemotherapy alone — has grown from 2.6 to 13.6%, and those who underwent chemo- and endocrinotherapy — has increased from 8.4% to 28.8%. The number of patients who did not receive adjuvant systemic therapy has significantly decreased (68.3% before 1995, and 13.3% after 2005; p<0.05). The analysis of adjuvant chemotherapy regimens showed a significant increase of the number of patients with anthracycline-containing combinations of cytostatic agents (АС, FAC, FEC, etc) from 61.8% (before 1995) to 84.6% (after 2005); since 2005 adjuvant regimens with taxanes (docetaxel and paclitaxel) have been introduced into practice — 5.3%; sequential or single-step anthracycline and taxane combinations were administered to 4.9% patients treated after 2005. The number of women who received anthracycline-free combinations (CMF) has decreased significantly — from 38.2% (before 1995) to 5.2% (after 2005), p<0.05. HER2-status determination was introduced into practice after 2000; however, adjuvant trastuzumab therapy in HER2-positive breast cancer started being used only after 2005 (in 50.8% women with HER2-positive cancer). Adjuvant endocrinotherapy has also undergone significant changes for the past 25 years: the number of women receiving anti-estrogens (tamoxifen) alone has reduced from 84.2% (before 1995) to 52.4% (after 2005), p<0.05; since 2000 aromatase inhibitors and sequential administrations of tamoxifen and aromatase inhibitors have been used; the number of patients who underwent castration alone and had combined regimes (castration, tamoxifen) has not changed significantly in the course of time (p>0.05) (Table 3).
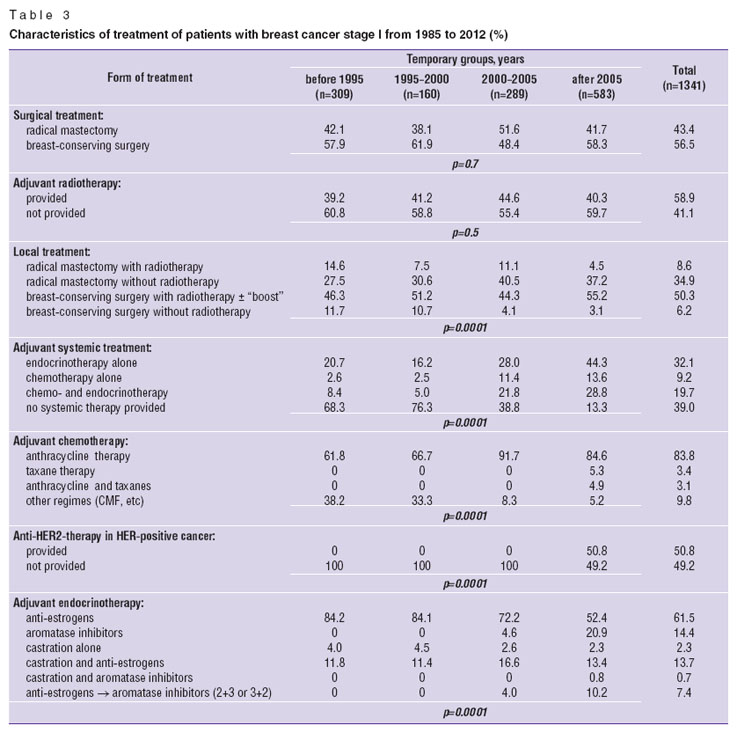 Table 3. Characteristics of treatment of patients with breast cancer stage I from 1985 to 2012 (%) Table 3. Characteristics of treatment of patients with breast cancer stage I from 1985 to 2012 (%)
|
Thus, over the past 27 years there have been revealed significant changes in the paradigm of the breast cancer stage I therapy: after 2005 radiotherapy became a compulsory element of conservation therapy, and in half of women (50.3%) it was accompanied with “boost” on a removed tumor bed. The number of patients who received radiotherapy after radical mastectomy has significantly decreased: from 14.6% (before 1985) to 4.5% (after 2005), p<0.05. Adjuvant systemic therapy of breast cancer was used recently in the great majority of patients (86.7%): there has significantly grown the number of patients who received endocrinotherapy (from 20.7 to 44.3%), chemotherapy (from 2.6 to 13.6%) or chemo- and endocrinotherapy (from 8.4 to 28.8%), p<0.05. Major changes in chemotherapy regimens have taken place: anthracycline-free regimens (CMF) have been replaced by anthracycline-containing combinations, and after 2005 — by taxanes. HER2-status determination has been used in clinical practice since 2000, and trastuzumab adjuvant therapy — since 2005; about half of patients with HER2-positive stage I breast cancer (50.8%) have received trastuzumab anti-HER2-therapy. The number of women received tamoxifen has decreased (from 84.2 to 52.4%; p<0.05) in favor of other regimens (aromatase inhibitors and sequential regimens). These progressive changes in the treatment of Russian women prove worldwide tendencies of surgical and systemic management evolution of breast cancer, the most common oncopathology of women.
Study Funding and Conflict of Interests. The study was not supported by any funds, and the authors have no conflict of interest to disclose.
References
- Gatta G., Trama A., Capocaccia R. Variations in cancer survival and patterns of care across Europe: roles of wealth and health-care organization. J Natl Cancer Inst Monogr 2013; 2013(46): 79–87, http://dx.doi.org/10.1093/jncimonographs/lgt004.
- Souza F.H., Polanczyk C.A. Is age-targeted full-field digital mammography screening cost-effective in emerging countries? A micro simulation model. Springerplus 2013 Jul 31; 2: 366, http://dx.doi.org/10.1186/2193-1801-2-366.
- Elkin E.B., Atoria C.L., Leoce N., Bach P.B., Schrag D. Changes in the availability of screening mammography, 2000–2010. Cancer 2013 Aug 13, http://dx.doi.org/10.1002/cncr.28305.
- Abrahamsson L., Humphreys K. A statistical model of breast cancer tumour growth with estimation of screening sensitivity as a function of mammographic density. Stat Methods Med Res 2013 Jul 9, http://dx.doi.org/10.1177/0962280213492843.
- Syed B.M., Green A.R., Paish E.C., Soria D., Garibaldi J., Morgan L., Morgan D.A., Ellis I.O., Cheung K.L. Biology of primary breast cancer in older women treated by surgery: with correlation with long-term clinical outcome and comparison with their younger counterparts. Br J Cancer 2013 Mar 19; 108(5): 1042–1051, http://dx.doi.org/10.1038/bjc.2012.601.
- Rodríguez-Spiteri Sagredo N., Martínez Regueira F., Olartecoechea Linaje B., Arredondo Chaves J., Cambeiro Vázquez M., Pina Insausti L.J., Elizalde Pérez A., Garíca-Lallana A., Sola Gallego J.J. Accelerated partial breast irradiation with multicatheters during breast conserving surgery for cancer. Cir Esp 2013 Jul 1, http://dx.doi.org/10.1016/j.ciresp.2013.02.016.
- Skandarajah A.R., Bruce Mann G. Selective use of whole breast radiotherapy after breast conserving surgery for invasive breast cancer and DCIS. Surgeon 2013 Apr 27, http://dx.doi.org/10.1016/j.surge.2013.03.005.
- Murphy J.O., Sacchini V.S. New innovative techniques in radiotherapy for breast cancer. Minerva Chir 2013 Apr; 68(2): 139–154.
- Holleczek B., Jansen L., Brenner H. Breast cancer survival in Germany: a population-based high resolution study from saarland. PLoS One 2013 Jul 31; 8(7): e70680, http://dx.doi.org/10.1371/journal.pone.0070680.
- Hernandez-Aya L.F., Gonzalez-Angulo A.M. Adjuvant systemic therapies in breast cancer. Surg Clin North Am 2013 Apr; 93(2): 473–491, http://dx.doi.org/10.1016/j.suc.2012.12.002.
- Hickey B.E., Francis D.P., Lehman M. Sequencing of chemotherapy and radiotherapy for early breast cancer. Cochrane Database Syst Rev 2013 Apr 30; 4: CD005212, http://dx.doi.org/10.1002/14651858.CD005212.pub3.
- Pestalozzi B.C., Holmes E., de Azambuja E., Metzger-Filho O., Hogge L., Scullion M., Láng I., Wardley A., Lichinitser M., Sanchez R.I., Müller V., Dodwell D., Gelber R.D., Piccart-Gebhart M.J., Cameron D. CNS relapses in patients with HER2-positive early breast cancer who have and have not received adjuvant trastuzumab: a retrospective substudy of the HERA trial (BIG 1-01). Lancet Oncol 2013 Mar; 14(3): 244–248, http://dx.doi.org/10.1016/S1470-2045(13)70017-2.
- Kurian A.W., Lichtensztajn D.Y., Keegan T.H., Leung R.W., Shema S.J., Hershman D.L., Kushi L.H., Habel L.A., Kolevska T., Caan B.J., Gomez S.L. Patterns and predictors of breast cancer chemotherapy use in Kaiser Permanente Northern California, 2004–2007. Breast Cancer Res Treat 2013 Jan; 137(1): 247–260, http://dx.doi.org/10.1007/s10549-012-2329-5.