The Use of Hydrogel Materials Coletex-ADL and Colegel in the Treatment of Purulent Frontal Sinusitis
The aim of the investigation was to assess the treatment efficacy of purulent frontal sinusitis including local use of Russian hydrogel materials with antiseptic, analgesic and hemostatic properties in combination with sinus obliteration by osteoplastic materials and physiotherapy.
Materials and Methods. The study involved 20 subjects who had been operated on for destructive changes of frontal sinus walls due to purulent frontitis. For local treatment we used Russian depot-materials: hydrogel medical compositions based on biopolymer — sodium alginate. Intraoperatively we sanitated frontal sinuses: using hydrogel matrix Colegel with dioxydine and ε-aminocaproic acid we lined sinus walls and bone defect area at the level of operative approach after obliteration by osteoplastic composition МК-9М. A postoperative wound was blindly sutured and covered by hydrogel textile-biopolymer-based Coletex-ADL napkin with dioxydine and lidocaine. Magnetotherapy was being carried out since first postoperative days.
Results. Local intra- and postoperative use of hydrogel materials in combination with sinus obliteration by osteoplastic material and magnetotherapy since the first postoperative days contributed to the healing of frontal area wounds by primary adhesion within an optimal period. We recorded no complications and adverse sequelae of surgical interventions, hospital stay decreased by 7–10 days.
Conclusion. The use of Russian hydrogel materials — Colegel and Coletex-ADL matrices with antiseptics, anesthetic and hemostatic agents combined with sinus obliteration by osteoplastic materials contributes to the prevention of complications, reduction of the treatment period of patients with destructive changes of frontal sinus walls in inflammatory processes.
Currently, choosing pathogenetically reasonable and effective systemic and local therapy regimens in the treatment of purulent obstructive and prevention of purulent septic complications is no easy matter. It is conditioned by an increase in the resistence of microflora to antibiotic drugs, as well as changes in immunoreactivity, allergization of the population against the background of general environmental deterioration [1, 2].
The treatment efficacy of purulent inflammatory diseases including ENT diseases, can be significantly improved through the development of more precise diagnosis and treatment techniques, new methods of surgical intervention and postoperative treatment aimed at suppressing the inflammatory response of tissues, stimulating their necrolysis, and sanation. A closed method with the use of various dressings is optimal in terms of therapeutic and protective effect, creation of a required microclimate in the postoperative cavity [3, 4].
There are quite a number of treatment regimens of purulent sinusitis, which have their advantages and disadvantages. Thus, I.P. Vasilenko and M.P. Nikolaev’s method [5] provides frontal sinus obliteration by biocompatible implant material hydroxiapol and calapol with high osteoconductive and osteoinductive properties. During surgery, before the introduction of osteoplastic material into the cavity of the frontal sinus it is necessary to perform the removal of the mucous membrane, coagulation and sterilization of the frontal sinus walls with ther use of air plasma flow, the output temperature of which being from 3000° to 3500°C. The disadvantage of this method is that the degradation of the posterior and frontal walls of the orbital sinus that results in brain tunic exposure may lead to penetrating into the cranial cavity, damaging the brain and its meninges.
Another currently used method of surgical treatment of frontitis [6] implies opening the frontal sinus and anterior ethmoidal labyrinth cells with subsequent grafting of the frontonasal ostium with a nasal mucous membrane graft, grafting being carried out with a flap from the superolateral nasal wall which has a frontal base.
The disadvantage of this method in frontitis with posterior wall defects of the frontal sinus is that the defect closure of a sinus wall is to be performed with a mucous pedicle flap taken from the superolateral nasal wall. The flap is passed through the frontal ostium and serves as a protective layer between the sinus and the cranial cavity. Further you can perform obliteration of the frontal sinus cavity by osteoplastic composites aimed at stopping the spread of infection from the latter into the surrounding tissue, preventing liquorrhea development. However, after filling the sinus cavity with osteoplastic materials, mucous flap compresing by the hardening composite occurs which is accompanied by flap trophic damage and distruction.
A more sparing method, with a lower risk of inflammatory complications, is the method that provides frontal sinus obliteration by osteoplastic composition MK-9M (Russia). It was suggested in 2006 for the treatment of chronic destructive post-traumatic frontal sinusitis, frontal sinus giant osteomas with wall destruction and cranial cavity invasion. The adhesive osteoplastic composition MK-9M, when filling the sinus, hardens in 10–15 minutes. This time is enough to model the frontal and orbital surfaces of the sinus in the defective area with the elimination of communication with the cranial cavity or orbit [7]. A disadvantage of this method is a risk of toxic effects on the intracranial anatomical structures adjacent to the defect in the posterior sinus wall. Besides, when hardening, the osteoplastic composition slightly increases in volume and can prolapse into the cranial cavity, providing a chemical and compressing effect on the intracranial structures.
All the abovementioned shows that the search for new treatments of frontal sinusitis remains relevant.
The aim of the investigation was to assess the treatment effectiveness of purulent frontal sinusitis including local use of Russian hydrogel materials with antiseptic, analgesic and hemostatic properties in combination with sinus obliteration by osteoplastic materials and physiotherapy.
Materials and Methods. A new method of treatment in injuries of the frontal sinus walls, recurrent purulent and purulent polypous frontitis with the destruction of the frontal sinus walls, with its approbation in experiment and clinical practice, has been developed. The method includes making an access to the frontal sinus in a typical place (Fig. 1).
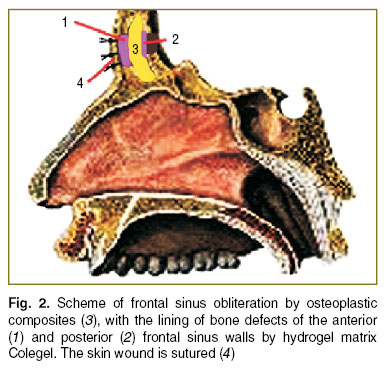
Then the sinus is sanitized, the area of the bone defect is lined by hydrogel matrix Colegel with ε-aminocaproic acid and Dioxydinum. After sinus obliteration by osteoplastic composition MK-9M (Fig. 2), the access place is lined by the same hydrogel matrix, over which the wound is sutured blindly and covered by a hydrogel textile-biopolymer-based Coletex-ADL napkinwith dioxydine and lidocaine.
When the sinus was being obliterated by the osteoplastic adhesive composition MK-9M, attention was paid to the sinus cavity being filled completely. Hardening of the composite material took 10–15 minutes, there was enough time to thoroughly model the frontal and orbital surface of the sinus in the defective area and eliminate communication with the intracranial cavity. These are the basics for the prevention of intracranial complications.
In addition, intravenous antibiotic therapy, desensitization, dehydration therapies were given in the postoperative period. In order to reduce inflammation, stimulate reparative processes, magnetic therapy with the Carnelian-1002 apparatus (Russia) (frequency of 1.4–1.5 Hz per minute, amplitude of 200 mT, a continuous regimen of 5–10 min every 2–3 days) was given early after surgery (in 6 h). Dressing was performed on the second day after surgery and further as indicated.
The given method was used to treat 20 subjects (main group) with destructive changes of the frontal sinus walls in inflammatory processes.
The comparison group included 35 subjects with purulent frontotomy who underwent surgery and postoperative treatment with a standard regimen. Trepanation of the anterior wall of the frontal sinus was performed by Ogston-Luke followed by sanitation and drainage of the frontal sinus. The postoperative wound was managed in the open way with daily cleaning with antibiotic and loose swabbing by anapkin soaked in solcoseryl gel or other reparants. Further, the wound surface was gradually filled with granulation tissue, healed by secondary intention.
Results and Discussion. Postoperative complications and unfavourable effects of the surgery were not observed in the study group. This was mainly due to the achievement of thorough hemostasis and elimination of the inflammatory cavity resulting from the intraoperative application of hydrogel matrix Colegel impregnated with antiseptic and hemostatic agents in combination with sinus obliteration by osteoplastic composition MK-9M.
Local treatment of the postoperative wound with the use of a Coletex-ADL napkin with lidocaine anesthetic and dioxydinum antiseptic provided absorbing, antibacterial, anti-inflammatory and analgesic effects. Pain relief in the wound within 6–12 hours after surgery or dressing, which are characterized by the greatest pain impulsing, should be attributed to the major advantages of these napkins. Additional administration of anaesthetics against the background of using Coletex-ADL napkins was not needed. The patients in the comparison group were administered oral or parenteral anaesthetics for 2–5 days immediately after the surgical intervention (Fig. 3).
 Fig. 3. Duration of pain syndrom and inflammatory changes in the surgical wounds in the observation groups Fig. 3. Duration of pain syndrom and inflammatory changes in the surgical wounds in the observation groups
|
In the main group all the wounds in the frontal area healed on days 6–7 by primary intention with the formation of a soft elastic scar without signs of inflammation. The first dressing was performed on day 2 after surgery, further — as indicated. 2.3 dressingswere performed in each patient on average.
In the comparison group scarring and epithelialization of the wound surface were identified by days 14–17. Two cases of a complicated postoperative course in the form of frontal bone osteitis with fistula formation were registered. On average, 10.4 dressings were performed in each patient. (Fig. 4).
 Fig. 4. Healing time and hospital length of stay in the observation groups Fig. 4. Healing time and hospital length of stay in the observation groups
|
Thus, the use of hydrogel materials Coletex-ADL and Coletegel in combination with low frequency magnetic therapy during frontal sinus surgery in purulent sinusitis provides a reduction in the number of dressings and treatment costs, improves quality of life of patients, reduces the time of wound healing and hospital length of stay by one week on average.
Case history.
Patient Z., a 67 year old female, was urgently admitted to the otorhinolaryngology department, complaining of severe headaches, and the temperature up to 37.4°C, which she had had within a week. In the history: the patient had had a frontal lobe injury in a road accident 5 months before. She arrived at the otorhinolaryngology department on her own. She wasadvised by maxillofacial surgeons, neurosurgeons, otorhinolaryngologists and hospitalized with the diagnosis “chronic posttraumatic frontal sinusitis, exacerbation”. On examination, an infiltrate in the projection of the right frontal sinus was detected, being soft on palpation, painless, the skin over the latter was not changed.
A CT scan of the accessory nasal sinuses was performed, the frontal sinuses and anterior ethmoidal labyrinth cells on the right were found to be filled with a liquid soft-tissue content, the anterior and posterior walls of the frontal sinuses destructed (Fig. 5).
The patient was given advice by a physician, neurologist, ophthalmologist. ECG was taken, laboratory blood test and urinanysis were made. The patient gave her consent to surgical treatment. In the operating room, under general anesthesia, the incision into the typical area was made.
Musculocutaneous flap separation was performed, a soft tissue formation in the projection of the right frontal sinus anterior wall was exposed, the latter thoroughly removed by a blunt technique. When opened on the operating table, a cavity containing pus was detected, and the material was taken for histological examination.
On removing the suppurative encysted formation (possibly, an infected formed hematoma) the destructed posterior wall of the frontal sinus was exposed. Sinus sanitation was performed. Then the defect of the sinus posterior wall was lined by hydrogel matrix Colegel with previously introduced dioxidine and ε-aminocaproic acid. Further, the frontal sinus cavity was filled with adhesive osteoplastic composition MK-9M. While the hardening of the composite material, the sinus frontal and orbital surfaces in the area of the defect were modeled, and communication with the cranial cavity was eliminated. Aftersinus obliteration by the osteoplastic material the place of access was covered by the the same matrix, the wound being sutured blindly over it.
Postoperatively, the patients underwent intravenous antibiotic therapy, desensitization, dehydration therapy. Magnetic therapy with the Serdolik-1002 apparatus started 6 h after the operation.
The postoperative period was unremarkable. The wound healed by primary intention. After repeated examinations by the therapist, neurologist, ophthalmologist, laboratory tests, CT scan, obtaining the results of histological examination, the patient was discharged on day 7 for domiciliary outpatient aftercare in satisfactory condition (Fig. 6).
In the course of frontal sinus intervention on purulent sinusitis the sinus walls and the defects in them were lined by hydrogel matrix Colegel with preinjected dioxidine and ε-aminocaproic acid.
The effectiveness of the surgical intervention was achieved by antiseptic and hemostatic properties of the hydrogel material. The sodium alginate biopolymer-based matrix Colegel also performs stimulating and protective functions and prevents prolapsing the osteoplastic composition into the cranial cavity and under the skin like a “corset”. The elimination of a pathological inflammatory cavity, the communication of the frontal sinus with the anterior cranial fossa and orbit was achieved by sinus cavity obliteration by adhesive osteoplastic composition MK-9M.
Started since the first day after surgery, magnetic therapy stimulates reparative processes through anti-inflammatory, antiedematous and antiseptic effects. Though, magnetotherapy also provides desagragation and hypocoagulation impact that may cause bleeding, that is why in the suggested method, ε-aminocaproic acid was injected into matrix Colegel to enhance a hemostatic effect by preventing fibrinolysis.
The effectiveness of the suggested method of purulent sinusitis treatment is emphasized by the absence of complications and unfavourable results of surgical intervention, acceleration of postoperative wound healing and hospital stay reduction by 7–10 days.
Conclusion. The presented purulent frontitis treatment method, which includes local intra- and postoperative use of hydrogel materials Colegel and Coletex-ADL impregnated with antiseptic, hemostatic and anesthetic agents, in combination with the obliteration of the sinuses by osteoplastic materials reduces the need for parenteral administration of drugs, thus reducing the risk of sensitization of the patients, development of toxic effects against the background of drug therapy, the length of hospital stay by one week on average and ensures prevention of suppurative complications. Magnetic therapy since the first day after surgery promotes frontal lobe wound healing by primary intention at the optimal time.
Study Funding and Conflict of Interests. The study was not funded by any sources, and there are no conflicts of interest related to the present study.
References
- Martinez-Beneito M.P., de la Fuente Arjona L., García Callejo F.J., Mallea Cañízares I., Blay Galaud L., Marco Algarra J. Subdural empyema of sinus origin caused by Gemella morbillorum, a strange etiology. Acta Otorrinolaringol Esp 2002; 53(6): 427–430.
- Wald E. R. Beginning antibiotics for acute rhinosinusitis and choosing the right. Clin Rev Allergy Immunol 2006; 30(3): 143–152.
- Abaev Yu.K. Current characteristics of surgical infection. Vesti khirurgii 2005; 164(3): 107–111.
- Khar’kova N.A., Gerasimenko M.Yu., Oltarzhevskaya N.D., Egorova E.A. Computed tomography in the control of hydrogel depot-materials used to treat purulent maxillary sinusitis. Radiologiya — praktika 2014; 1: 24–31.
- Vasilenko I.P., Nikolaev M.P. Sposob obliteratsii lobnoy pazukhi [Frontal sinus obliteration technique]. Patent RF No.2476171. 2010.
- Yanborisov T.M. Sposob khirurgicheskogo lecheniya frontita [Frontal sinusitis surgery technique]. Patent RF No.2118512. 2007.
- Khar’kova N.A. Vozmozhnosti i perspektivy khirurgicheskoy obliteratsii lobnykh pazukh kleevoy osteoplasticheskoy kompozitsiey MK-9M. Dis. … kand. med. nauk [Capabilities and prospects of surgical obliteration of frontal sinuses by adhesive osteoplastic composition МК-9М. Dissertation for the degree of Candidate of Medical Sciences]. Moscow; 2006.