The Possibilities of Modern Methods of Oxidative Stress and Immune Profile Study in Determining the Predictors of Chronic Inflammatory Process in the Bronchi of Young Beginning Smokers
The aim of the investigation was to assess the possibilities of the modern methods for oxidative stress and immune profile research in determining the predictors of chronic inflammatory process in the young smokers bronchi.
Materials and Methods. 85 students of the I–III-year from Nizhny Novgorod State Medical Academy were examined, among them 30 students (group 1) were non-smokers and 55 students (group 2) were addicted to nicotine. The pulmonary function test, oxidant–antioxidant system, the levels of soluble differentiating molecules of leucocytes and histocompatibility molecules were studied along with general clinical examination methods. Only students with normal pulmonary function test indices were included in the study.
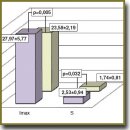
Results. Antioxidant system activation and decreasing intensity of lipid peroxidation was characteristic of young smokers. Thus, statistically significant increase in erythrocytes superoxide dismutase was revealed in group 2, and the indices of maximum luminescence intensity Imax and S light sum were decreased. The smokers showed significant increase in sCD95 apoptosis modulator, growing content of sCD25 and sCD8 immune cells activation markers, growing total fraction of sCD54 adhesion molecules as well as soluble histocompatibility molecules of class I and II.
Conclusion. At the first stages smoking is accompanied by compensatory immune reactions, antioxidant system activation, as well as decreasing lipid peroxidation intensity. Modern methods of researching oxidant–antioxidant system as well as the levels of differentiation and histocompatibility molecules allow studying the subtle mechanisms of smoking impact on the respiratory system at the “pre-obstructive” stage and tracing the appearance of chronic bronchi inflammation predictors.
- Bova A.A., Lapitskiy D.V. Modern approaches to the diagnosis and treatment of ischemic heart disease in patients with chronic obstructive pulmonary disease. Meditsinskie novosti 2007; 9: 7–14.
- Global’naya strategiya diagnostiki, lecheniya i profilaktiki khronicheskoy obstruktivnoy bolezni legkikh (peresmotr 2011 g.) [Global strategy of diagnosis, treatment and prevention of chronic obstructive pulmonary disease (revised in 2011)]. Pod red. Belevskogo A.S. [Belevskiy A.S. (editor)]. Moscow: Rossiyskoe respiratornoe obshchestvo; 2012.
- Postnikova L.B., Kubysheva N.I., Boldina M.V., Li T.V., Klimanov I.A., Novikov V.V. Nitrous stress and soluble differentiation molecules in exacerbation of chronic obstructive pulmonary disease. Pul’monologiya 2012; 1: 35–39.
- Soodaeva S.K. The role of free-radical oxidation in COPD pathogenesis. Atmosfera. Pul’monologiya i allergologiya 2002; 1(4): 24–25.
- Garey K.W., Neuhauser M.M., Robbins R.A., Danziger L.H., Rubinstein I. Markers of inflammation in exhaled breath condensate of young healthy smokers. Chest 2004; 125(1): 22–26, http://dx.doi.org/10.1378/chest.125.1.22.
- Chuchalin A.G. Tobacco smoking and respiratory diseases. Russkij medicinskij zurnal 16(22): 1477–1481.
- Muravlyova L.E., Molotov-Luchanskiy V.B., Kluyev D.A., Demidchik L.A., Kolesnikova E.A. The role of oxidative stress in pathogenesis of chronic obstructive pulmonary disease. Advances in current natural sciences 2012; 9: 12–16.
- Lin J.L., Thomas P.S. Current perspectives of oxidative stress and its measurement in chronic obstructive pulmonary disease. COPD 2010; 7(4): 291–306, http://dx.doi.org/10.3109/15412555.2010.496818.
- Mishina N.A. The peculiarities of the oxidation stress formation in erythrocytes in the patients with chronic obstruction pulmonary disease. Aspirantskiy vestnik Povolzh’ya 2009; 7–8: 42–46.
- Dworski R. Oxidant stress in asthma. Thorax 2000; 55(Suppl 2): S51–S53, http://dx.doi.org/10.1136/thorax.55.suppl_2.S51.
- Park H.S., Kim S.R., Lee Y.C. Impact of oxidative stress on lung diseases. Respirology 2009; 14(1): 27–38, http://dx.doi.org/10.1111/j.1440-1843.2008.01447.x.
- Chuchalin A.G. Chronic obstructive pulmonary disease and comorbidities. Zdorov’ya Ukraini 2010; 3(232): 40–41.
- Boots A.W., Haenen G.R.M.M., Bast A. Oxidant metabolism in chronic obstructive pulmonary disease. Eur Respir J 2003; 22(Suppl 46): 14s–27s, http://dx.doi.org/10.1183/09031936.03.00000403a.
- Novikov V.V., Evsegneeva I.V. New human differentiation antigens adopted at the VII international workshop. Rossiyskiy bioterapevticheskiy zhurnal 2003; 2(3): 1–4.
- Novikov V.V., Karaulov A.V., Baryshnikov A.Yu. Rastvorimye formy membrannykh belkov kletok immunnoy sistemy [Soluble membrane proteins of immune system cells]. Moscow: MIA; 2008; 249 p.
- Siafakas N.M., Tzortzaki E.G. Few smokers develop COPD. Why? Respir Med 2002; 96(8): 615–624, http://dx.doi.org/10.1053/rmed.2002.1318.
- Burlakova E.B., Zhizhina G.P., Gurevich S.M., Fatkullina L.D., Kozachenko A.I., Nagler L.G., Zavarykina T.M., Kashcheev V.V. Biomarkers of oxidative stress and smoking in cancer patients. J Can Res Ther 2010; 6(1): 47–53, http://dx.doi.org/10.4103/0973-1482.63569.
- Torres-Ramos Y.D., Garcнa-Guillen M.L., Olivares-Corichi I.M., Hicks J.J. Correlation of plasma protein carbonyls and C-reactive protein with GOLD stage progression in COPD patients. Open Respir Med J 2009; 3: 61–66, http://dx.doi.org/10.2174/1874306400903010061.
- Jiao Z.X., Ao Q.L., Xiong M. Cigarette smoke extract inhibits the proliferation of alveolar epithelial cells and induces apoptosis. Sheng Li Xue Bao 2006; 58(3): 244–254.
- Scott D.A., Palmer R.M. The influence of tobacco smoking on adhesion molecules profiles. Tab Ind Dis 2002; 1(1): 7–25, http://dx.doi.org/10.1186/1617-9625-1-1-7.
- Pace E., Ferraro M., Di Vincenzo S., Bruno A., Giarratano A., Scafidi V., Lipari L., Di Benedetto D.V., Sciarrino S., Gjomarkaj M. Cigarette smoke increases BLT2 receptor functions in bronchial epithelial cells: in vitro and ex vivo evidence. Immunology 2013; 139(2): 245–255, http://dx.doi.org/10.1111/imm.12077.
- Aaron C.P., Schwartz J.E., Bielinski S.J., Hoffman E.A., Austin J.H., Oelsner E.C., Donohue K.M., Kalhan R., Berardi C., Kaufman J.D., Jacobs D.R. Jr., Tracy R.P., Barr R.G. Intercellular adhesion molecule 1 and progression of percent emphysema: the MESA Lung Study. Respir Med 2014; 109(2): 255–264, http://dx.doi.org/10.1016/j.rmed.2014.10.004.
- Lyubavina N.A., Varvarina G.N., Makarova E.V., Menkov N.V., Belyaeva E.V., Ermolina G.B., Presnyakova N.B., Korolyova V.V., Filatova E.N., Kurnickov G.Yu., Noviсkov V.V. Serous content of adhesion soluble antigen as a marker of the chronic obstructive pulmonary disease progressing. Sovremennye tehnologii v medicine 2011; 1: 67–71.
- Thichanpiang P., Wongprasert K. Green tea polyphenol epigallocatechin-3-gallate attenuates TNF-α-induced intercellular adhesion molecule-1 expression and monocyte adhesion to retinal pigment epithelial cells. Am J Chin Med 2015; 2: 1–17, http://dx.doi.org/10.1142/S0192415X1550007X.
- Bou Ghanem E.N., Clark S., Du X., Wu D., Camilli A., Leong J.M., Meydani S.N. The α-tocopherol form of vitamin E reverses age-associated susceptibility to streptococcus pneumoniae lung infection by modulating pulmonary neutrophil recruitment. J Immunol 2015; 194(3): 1090–1099, http://dx.doi.org/10.4049/jimmunol.1402401.
- Majo J., Ghezzo H., Cosio M.G. Lymphocyte population and apoptosis in the lungs of smokers and their relation to emphysema. Eur Respir J 2001; 17(5): 946–953, http://dx.doi.org/10.1183/09031936.01.17509460.
- Kubysheva N.I., Postnikova L.B., Presnyakova N.B., Novikov V.V. Participation of soluble major histocompatibility class i molecules in the development of chronic obstructive pulmonary desease. Vestnik Nizhegorodskogo universiteta im. N.I. Lobachevskogo 2010; 2(2): 541–543.
- Gorbunov N.V. Sostoyanie mikrososudistoy reaktivnosti i funktsii vneshnego dykhaniya u kuryashchikh studentov-medikov. Avtoref. dis. … kand. med. nauk [Microvascular reactivity and external respiratory function in smoking medical students. Abstract for Dissertation for the degree of Candidate of Medical Science]. Astrakhan’; 2013.










