The Development and Clinical Testing of “EXAR”, Passive Upper Limb Exoskeleton
The aim of the investigation was to develop and perform a clinical approbation of a modern passive upper-limb exoskeleton for the habilitation and rehabilitation of disabled patients with upper flaccid para(mono)paresis.
Materials and Methods. We performed a phase-by-phase anatomic parametrisation of an exoskeleton. We tested different exoskeleton designs made of different materials. Testing was also carried out on the various spring elements and rubber rings used as elastic elements. On the basis of the findings we created “EXAR”, a prototype passive exoskeleton for the upper limb. Testing of the design and the adaptation of its elements was carried out on 7 patients with upper para(mono)paresis syndrome.
Results. On comparing the materials for possible use in the “EXAR” exoskeleton we preferred magnesium-aluminium alloys and the use of rubber rings for its elastic elements. During the design and production of this exoskeleton we observed a modular principle. In use we were able to note that the “EXAR” passive exoskeleton increased the range of movement in the shoulder and elbow joints, this being a key requirement for the device in addition to its effect on habilitation and rehabilitation.
Conclusion. We consider the results of approbation of the “EXAR” passive exoskeleton for the upper limb to be positive, but that they indicate a requirement for further development and modernisation.
An analysis of the literature did not reveal any information about the wide medical application of passive exoskeletons of the upper limbs in our country or in Europe. Data about this kind of device can be found mainly from the USA, although such information usually concerns military applications [1, 2], however, there is an undoubted need for exoskeletons in practical healthcare.
The role of the upper limbs in daily life cannot be overestimated: they are indispensable for full-scale exploration of the world by children and for the active independent activity by adults. And while people disabled through impairment of their lower limbs can be provided with some means of assisting mobility (walkers, wheelchairs, special cars), there is not yet an adequate systemic technical solution [3] for patients with upper limb para(mono)paresis, despite many attempts to implement such solutions.
The aim of the investigation was to develop and perform a clinical testing of a modern passive upper limb exoskeleton for the habilitation and rehabilitation of disabled patients with flaccid upper limb para(mono)paresis.
The study addressed the following tasks:
identifying the requirements for a passive exoskeleton, “EXAR”, and determining its optimal technical characteristics;
during the testing evaluating and selecting the optimal materials for manufacturing the device;
developing methods of anatomic parametrisation in the application of the device;
determining the indications and contra-indications for the use of the “EXAR” exoskeleton;
identifying the possibilities of the device in compensating for the lost limb-functions.
Materials and Methods
Design of the study. Our initial attempts to perform mathematical modelling of the designs we had developed were unsuccessful and have been left for future investigation, as we discovered that such modelling required knowledge of a number of parameters — the weight of the upper limb and the power of its muscles, and to obtain absolute values for these is currently not possible.
Initially we used time-consuming methods of empirical selection of various options in trying to determine the inverse relationships, but we were unable to achieve stable operation of the designs. We therefore needed to develop a method of phase-by-phase anatomical parametrisation of the device [4–6].
Anatomical parametrisation is the determination of correlations between different anatomical characteristics of the human body and the parameters of the mechanical device in order to ensure the optimal operation of the resulting biomechanical system. The following stages are involved in anatomical parametrisation [6]:
stage 1 — defining the points for anatomical markers on the patient;
stage 2 — determination of any linear anatomical dimensions required for further analysis and calculations;
stage 3 — determination of the anatomically dependent parameters of the device which affect its capacity to compensate for the lost functions of the upper limb;
stage 4 — determination of the optimal relationships between the device and the limb that are required to achieve normal operation to substitute for the lost functions (priority for the Patent of the Russian Federation dated 16 March 2016, registration number 2016109511 of the Federal Service of the Russian Federation for Intellectual Property, Patents and Trade Marks).
The requirements for the “EXAR” passive exoskeleton were developed by analysing the biomechanics of the main movements of the upper human limb [7].
We tested the following materials during manufacture: Bakelite plywood, aluminum alloys Al-Mg3, Al-Mg5, Al-Mn and Al-Сu-Mg, medical stainless steel, PLA- and ABS-plastic, two-component JETACAST 70 injection moulded plastic, orthopedic low-temperature thermoplastics with shape memory: Turbocast and Polivik, rigid fix-polymers, and poly-ester and epoxy resins. Domestically-manufactured materials were preferred.
The following production methods were tested for the components: 3D modelling, digitally-controlled 3D milling, 3D printing, cast-moulding, and laser cutting.
Different types of springs and rubber rings were evaluated as elastic components.
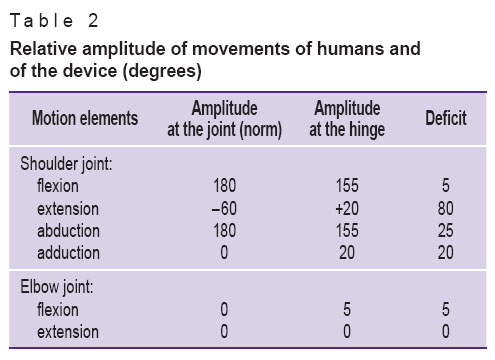
The device was tested and adapted to suit 7 patients with upper para(mono)paresis (Table 1), randomly selected from a database of such patients (59 individuals). The investigation was performed in accordance with the Helsinki Declaration (accepted in June 1964 (Helsinki, Finland) and reviewed in October 2000 (Edinburgh, Scotland)). The protocol of the investigation was coordinated with the Regional Ethical Committee of the Volgograd Medical Research Centre. An informed consent was obtained from the patient or from their parents in each case.
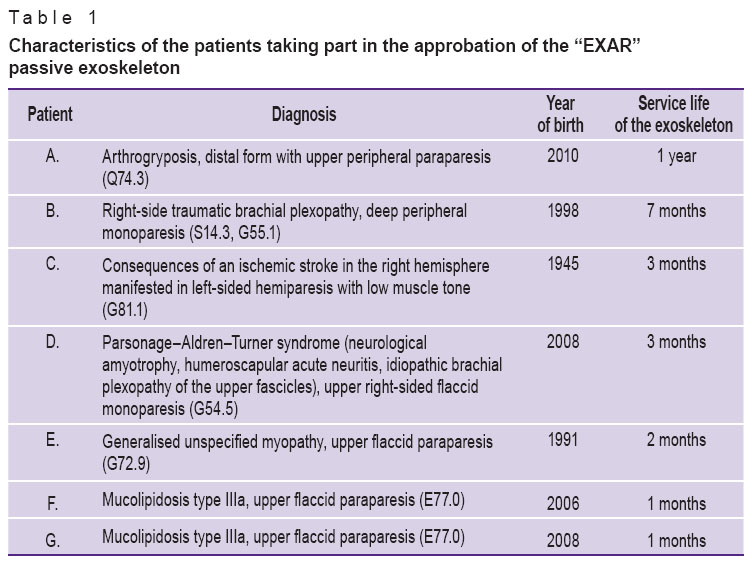 Table 1. Characteristics of the patients taking part in the approbation of the “EXAR” passive exoskeleton Table 1. Characteristics of the patients taking part in the approbation of the “EXAR” passive exoskeleton
|
To determine the effectiveness of using the “EXAR” passive exoskeleton we compared the amplitudes of active movements of the upper limbs without the device (this initial level was taken as a reference level) and immediately after putting the exoskeleton on the patient. In the absence of a standardised method for testing a passive upper limb exoskeleton the number and duration of the sessions were determined individually according to the principle of identifying the subjective minimal load and recording its gradual increase, under the supervision of physiotherapists, taking into account the individual’s tolerance of exercise therapy. We consider that the widespread future use of the exoskeleton we have developed is impossible without developing a detailed validation of its method of use. The maximum period of follow-up monitoring of the indicators of active movements of the upper limb without the device was 1 year.
The indication for the patients to be listed in the database and for their inclusion in the study was flaccid para(mono)paresis syndrome resulting from any of the following diseases:
1) arthrogryposis;
2) infantile cerebral palsy (atonic-astatic form and those forms where there is mixed muscle tone with a predominance of hypotonia);
3) neural Charcot–Marie–Tooth disease;
4) spinal amyotrophy;
5) brachial plexopathy accompanied with thrombocytopenic Henoch–Schönlein purpura; injuries and birth traumas (“obstetric paralysis”); extra cervical ribs (“thoracic inlet” syndrome); as a result of the improper position of the upper limb under anesthesia during a prolonged operation period; associated with granulomatous vasculopathy initiated by Herpes zoster; or exogenous intoxication with dopamine;
6) Guillain–Barré syndrome;
7) Larsen syndrome;
8) Ehlers–Danlos disease;
9) diastrophic dysplasia;
10) congenital myopathy (“central core” disease, nemaline myopathy and other variants of “floppy infant” syndrome);
11) myotonic dystrophy;
12) amyotrophic lateral syndrome, anterior corneal form.
Use of the prototype device was indicated if there was a complex of symptoms of upper flaccid paraparesis manifested in the following ways:
reduced muscle power (flexors, extensors, pronators, supinators, abducting muscles, adducting muscles) of the upper limbs up to scores 1, 2 or 3, which correspond to a moderate or severe degree of paresis;
limited rate, volume (amplitude) of movement in proximal and distal parts of the upper limbs: limitation of or inability to perform flexion or extension of the arms in the shoulder and/or elbow joints; inability to raise the arm up to the shoulder girdle and higher; inability to move the arm away from the body; limitation of or inability to rotate the upper limb;
reduced muscle tone in the proximal and distal parts of the upper limbs or mixed tone with a prevalence of hypotonia;
reduced or lack of tendon jerks in the arms (flexion-elbow, extensor-elbow, carporadial reflexes);
lack of contractures in the joints of the upper limb(s).
In this complex of symptoms there is anatomical-physiological separation between the central and peripheral nervous systems, with both direct connection and feedback being broken.
The inclusion criteria were the following: age over 3 years, normal level of mental development of children, lack of explicit cognitive deficit in adults, presence of upper flaccid (peripheral) moderate/severe mono/parapareses or upper mixed moderate/severe mono/parapareses with a prevalence of hypotonia.
The exclusion criteria and counter-indications for using the device were the following: age under 3, mental retardation of children, explicit cognitive impairment of adults, presence of spastic hypertonus of the muscles of the upper limbs, presence of contractures in large joints of the upper limbs, oncological diseases in incurable stages.
Results
Identification of the requirements for a passive exoskeleton of the upper limbs. Our analysis of the typical principal movements of an upper limb, those most frequently used in the everyday life of a healthy human, allowed us to determine a set of movements and their amplitudes required for self-service and for the full physical development of a disabled person that should be achievable when using the “EXAR” passive exoskeleton. As a result of this we formulated the requirements which the device should meet:
it should have a range of motion close to that of a healthy person;
it should have a light and durable construction adjusted to the anatomical parameters of the limb;
the construction components should replicate the shape of the human upper limb;
it should be made of biologically inert materials;
it should provide the possibility to remove and change structural components as a child grows;
it should be affordable for the mass market [8];
it should be mobile and be independent of external power sources;
it should not depend on foreign components.
The safety criteria set for the tested device were as follows: lack of electrical wires, unlimited freedom of movements within physiological norms; lack of sharp corners and edges in its construction; lack of any extra load on the joints; those parts of the device which are in contact with the patient’s body must be made of materials permitted for medical use in the Russian Federation.
Technical characteristics of the prototype “EXAR” exoskeleton. We produced and tested two basic versions of passive exoskeleton — fixed, attached to a wheelchair, and mobile, attached to a bespoke jacket.
The weight of the “EXAR” exoskeleton, along with the jacket, for a child with paraparesis is 1,200–1,800 g depending on the body weight; that for an adult patient with paraparesis — 2,000–2,200 g. For the patients with monoparesis the device is lighter. The fixed model of the device is lighter than the mobile one, as it does not include a jacket.
It should be noted that the weight of the final device was greater than that of the initial version made on a 3D printer as a result of replacing the plastic with magnesium-aluminium alloy and the introduction of some bearing assemblies. As a result, there were benefits in the strength and durability of the device.
The prototype version of the exoskeleton can move in three planes: sagittal, frontal and horizontal (intermediate and optimal plane). Rotational movements are not provided for in this device. The comparative amplitude of movements is provided in Table 2.
|
|
Cost calculation for the “EXAR” exoskeleton places it in the category of affordable exoskeletons [8]. The findings show that the deficit in movements in the device is not very significant and that its hinges allow quite adequate reproduction of the normal movements of the upper limb.
During the development and approbation of the different versions of the “EXAR” device it was determined that it is impossible to find an optimal solution if the following requirements are not met.
1. Preference given to the use of magnesium-aluminium alloys, because they have an optimal combination of lightness and durability, although its processing is intensive and specific.
2. During assembly of the elastic components of the device it is more effective to use rubber rings, as they do not require complex adjustment unlike springs, and the patient can individually select the number required.
3. For determining the optimal leverage of the device special attention should be paid to the selection of rods for the shoulder girdle and shoulder. If rotation of the forearm is impaired, the splint should be set individually.
4. To increase the durability of the pivots should be incorporated (32 in total for the device).
5. To provide an opportunity to change the elements of the device depending on a child’s height and any deterioration (deformation) of the elements it is necessary to divide the parts of the exoskeleton into those that are anatomically dependent and the ones that are anatomically independent.
6. For designing and producing the exoskeleton it is necessary to use a modular principle. This significantly widens the possibilities of the construction and presupposes some adjustments of the device and the use of supplementary elements, providing for involvement of the wrist joint and rotational functions of the impaired limb.
Clinical testing. The investigation into the potential of the “EXAR” exoskeleton involved 7 patients (See Table 1). The procedure involved activities with and without the device at a medical-sports complex and in everyday use at home, in kindergartens, during games, routine work and self-care (eating, hair-combing, washing, cleaning teeth etc.). The use of the “EXAR” passive exoskeleton had the following positive effects:
1. Increased amplitude of movement in the shoulder and elbow joints. This effect is the key one for the device. It was determined that in all cases the use of the “EXAR” exoskeleton contributed to increased amplitude of movements in shoulder and elbow joints. To a certain extent the operational amplitude of possible movements with the device, if there are no contractures of the upper limbs, can be determined before the use of the device by identifying the difference between the residual active and passive movements of the upper limb. Thus, if there is no muscle and joint stiffness the increased range of limb movement can reach the predetermined amplitude of movements provided by the passive exoskeleton itself.
2. Effect of habilitation. This effect is connected with the increased amplitude of movements. Our results showed that functionality of the upper limb(s) increased considerably. Using the terminology of Kapandzhi [7] one can state that if there are no contractures in the limbs the device allows the full use of the front counter-lateral movements, partial use of the front homo-lateral movements and partial use of rearward movements. The partial limitations of the two latter types of movement is caused by the lack of a possibility for rotational movements within the device. However, without the device it would be very difficult to use these types of movements at all. Therefore, the patient has the opportunity to perform everyday functions involved in self-care, such as personal hygiene, and eating, as well as the chance to recover lost skills such as playing the piano, drawing, and dancing involving the use of the arms (Figures 1, 2).
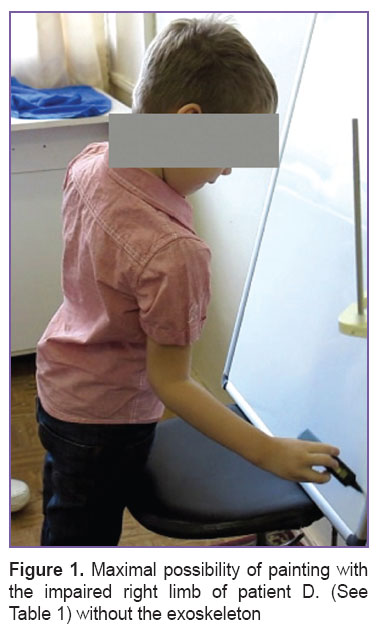 Figure 1. Maximal possibility of painting with the impaired right limb of patient D. (See Table 1) without the exoskeleton Figure 1. Maximal possibility of painting with the impaired right limb of patient D. (See Table 1) without the exoskeleton
|
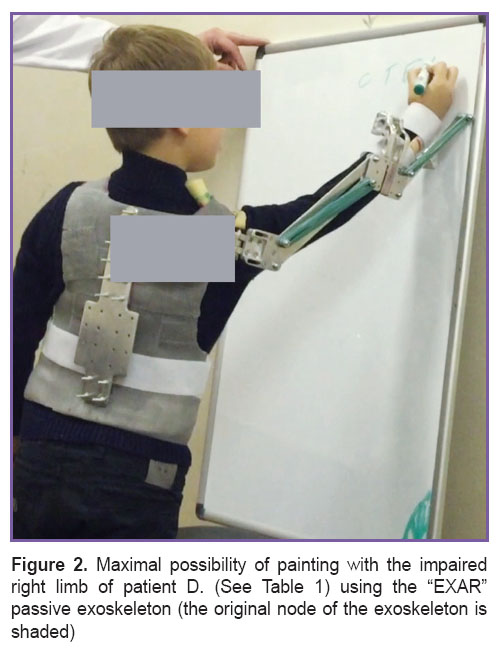 Figure 2. Maximal possibility of painting with the impaired right limb of patient D. (See Table 1) using the “EXAR” passive exoskeleton (the original node of the exoskeleton is shaded) Figure 2. Maximal possibility of painting with the impaired right limb of patient D. (See Table 1) using the “EXAR” passive exoskeleton (the original node of the exoskeleton is shaded)
|
3. Effect on rehabilitation. This issue has yet to be studied sufficiently and is to be the subject of further investigation. To provide more detailed answers the follow-up period needs to be extended (1 year or more). Furthermore, it would be necessary to evaluate the likely course of the disease causing the paresis of the upper limbs. However, results of the long-term observation (1 year) of the patient with arthrogryposis (patient A. in Table 1) is optimistic. The amplitude of movements of the upper limb of this patient were considerably increased with the use of the “EXAR” exoskeleton (Table 3).
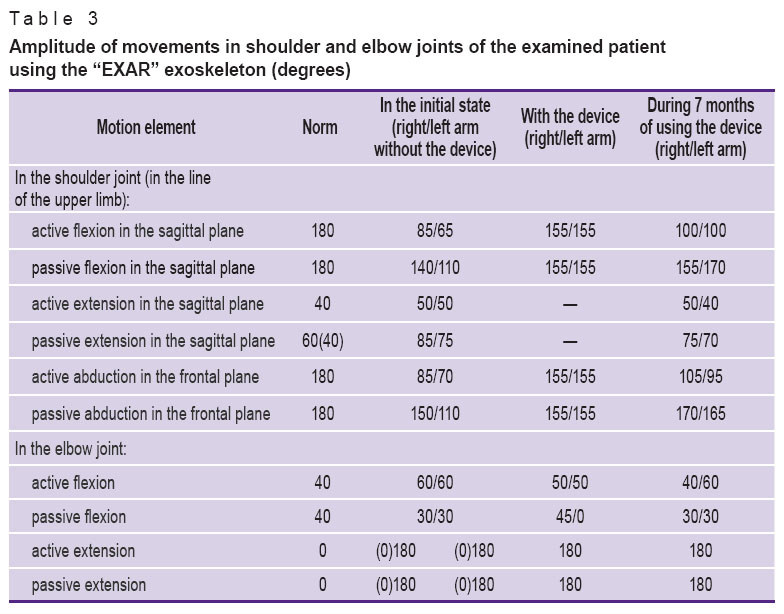 Table 3. Amplitude of movements in shoulder and elbow joints of the examined patient using the “EXAR” exoskeleton (degrees) Table 3. Amplitude of movements in shoulder and elbow joints of the examined patient using the “EXAR” exoskeleton (degrees)
|
We suppose that the effect of rehabilitation is based on biofeedback. Treatment with biofeedback techniques have proved the rationality of this, as adaptive brain systems are activated against the background of development of pathological processes in the CNS. Taking into account that the “core” of the clinical picture of the diseases we studied is flaccid paresis of the upper limbs, and the main factor involved in their development is damage, from various origins, to the nervous system, resulting in the impairment of direct connection and feedback between its central and peripheral parts, it is logical to treat the mechanisms of their restoration. The medical treatment of these pathologies is aimed mainly at restoration of the direct connections between the CNS and the peripheral system. Such restoration of feedback between the peripheral and central nervous systems is a task solved mainly with physiological procedures, massages and physiotherapy. The exoskeleton, in our opinion, provides an ideal way for the restoration of feedback. It helps influence, safely, the classic reflexogenic-receptor muscle areas and tendons of the upper limbs and restores the activity of the reflex arcs sending information about movements to the corresponding segments of the spinal cord. The spinal cord in its turn activates the “silent” motor cortex through its ascending pathways. According to neurophysiological laws, by restoring biofeedback between the periphery and the central parts of the central nervous system we can contribute to the enhancement of the direct effect of the CNS on the peripheral nervous system, as the mechanisms of self-regulation become involved. Thus, we can perform non-medical correction of the pathological development of the nervous system, as the volumes, rates and amplitudes of movements in the upper limbs are increased. It is also undeniable that if there is full mobility in the joints of the upper limbs, the probability of muscle and joint contractures will be limited.
4. The effect of prevention of posture disorders. This effect is connected with the carrying-corset (jacket), which, apart from its main function, contributes to the correction of posture disorders, preventing hyperlordosis, as other back muscles are involved in the process of arm-raising.
Analysis of our results leads us to consider that the “EXAR” passive exoskeleton for the upper limbs completely meets its clinical-anatomical requirements, allows for full reproduction of limb movements in its bearings in accordance with the normal movements of the upper limb, and provides for habilitation and rehabilitation of patients with upper para(mono)paresis. The beneficial effects of the device can be divided into two groups: early ones, connected with the immediate opportunity to widen the range of movements of the upper limb, and delayed ones connected with muscle training and elimination of the consequences of muscle and joint contracture, as well as with the prevention of hyperlordosis.
Conclusion. We consider the first experience of using the “EXAR” passive exoskeleton for the upper limb to be a positive one. The main direction for further experimental development today is the search for and implementation of new design solutions to widen the range of possible movements of the device to correspond to the normal range of movements of the upper limb in the shoulder and elbow joints and to determine the possibility of compensation for impaired functioning of the hand by involving movements in the wrist joint.
Study Funding. The study was funded with extra-budgetary sources from Volgograd State Medical University.
Conflicts of Interest. The authors have no conflicts of interest.
References
- Vorobyev A.A., Petrukhin A.V., Zasypkina O.A., Krivonozhkina P.S., Pozdnyakov A.M. Exoskeleton as a new means in habilitation and rehabilitation of invalids (review). Sovremennye tehnologii v medicine 2015; 7(2): 185–197, http://dx.doi.org/10.17691/stm2015.7.2.22.
- Ekzoskelet [Exoskeleton]. Vikipediya. URL: http://ru.wikipedia.org/?oldid=75908091.
- Rahman T., Sample W., Jayakumar S., King M.M., Wee J.Y., Seliktar R., Alexander M., Scavina M., Clark A. Passive exoskeletons for assisting limb movement. J Rehabil Res Dev 2006; 43(5): 583–590, http://dx.doi.org/10.1682/JRRD.2005.04.0070.
- Vorobev A.A., Andruschenko F.A., Zasypkina O.A., Krivonozhkina P.C. Methods of determining anatomically dependent parameters of the EХAR upper extremity exoskeleton. Volgogradskiy nauchno-meditsinskiy zhurnal 2015; 1: 58–61.
- Vorobev A.A., Andruwenko F.A., Zasypkina O.A., Krivonozhkina P.C. Features of anatomical parametrization of passive exoskeleton of upper extremity “EXAR”. Orenburgskiy meditsinskiy vestnik 2015; 3(4–12): 9–12.
- Voro’yev A.A., Andryushchenko F.A., Zasypkina O.A., Krivonozhkina P.S. Development of anatomical parameters of the upper limb exoskeleton “EXAR”. Zhurnal anatomii i gistopatologii 2015; 4(2): 27–30.
- Kapandzhi A.I. Verkhnyaya konechnost’. Fiziologiya sustavov [The upper limb. The physiology of the joints]. Moscow: Eksmo; 2014; 368 p.
- Vorobiev A.A., Andrutshenko F.A., Zasypkina O.A., Solovieva I.O., Krivonozhkina P.S., Pozdnykov A.M. Terminology and classification of exoskeleton. Vestnik Volgogradskogo gosudarstvennogo meditsinskogo universiteta 2015; 3(55): 71–78.