Relationship of Nutritional Status and Spirometric Parameters in Children with Bronchial Asthma
The potential mechanisms of bronchial asthma (BA) negative modification under the influence of obesity are currently being actively studied. However, at present, the effect of nutritional status on bronchial obstruction in children with BA cannot be considered established. In this regard, the purpose of this work was to study the relationship of spirometric parameters reflecting bronchial patency with nutritional status in children with asthma.
Materials and Methods. The study involved 54 patients with BA at the age of 8 to 17 years, 33 boys and 21 girls with different nutritional status. Assessment of nutritional status was carried out with the calculation of body mass index (BMI), relative body mass index (RBMI), and determination of body fat (% BF). Spirogram parameters were evaluated, including forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), FEV1/FVC ratio, maximum expiratory flow at the point of 25% loop flow-volume (MEF 25).
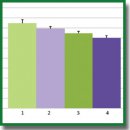
Results. Among the children examined, taking into account the BMI Z-score, 9.3% (5/54) had low body weight (group 1), 33% (18/54) had normal body weight (group 2), 31.5% (17/54) overweight (group 3), 25.9% (14/54) obesity (group 4). As the body weight increased, a statistically significant decrease in the FEV1/FVC ratio was observed, amounting to 84.6 [79.3; 90.0], 79.4 [76.6; 82.2], 74.6 [71.7; 77.5], 70.2 [67.0; 73.4]%, respectively, p=0.003; as well as a decrease in MEF 25 (% pred.), which amounted, respectively, to 95.6 [76.1; 115.2], 81.7 [71.4; 92.0], 56.3 [45.7; 66.9], and 48.4 [36.7; 60.1]%, p=0.003. A statistically significant negative relationship was found between indicators of nutritional status, including BMI, RBMI, % BF, and spirometry parameters reflecting bronchial patency, including FEV1/FVC ratio and MEF 25 (% pred.); all p<0.01.
Conclusions. Overweight and obesity in children with BA, estimated both by calculated methods with determination of BMI and RBMI and direct determination of body fat content, are accompanied by a statistically significant decrease in bronchial patency.
- GINA. Global strategy for asthma management and prevention. 2019. URL: https://ginasthma.org.
- Eliseeva Т.I., Balabolkin I.I. Modern technologies of bronchial asthma control in children (review). Sovremennye tehnologii v medicine 2015; 7(2): 168–184, https://doi.org/10.17691/stm2015.7.2.21.
- Braido F., Brusselle G., Guastalla D., Ingrassia E., Nicolini G., Price D., Roche N., Soriano J.B., Worth H.; LIAISON Study Group. Determinants and impact of suboptimal asthma control in Europe: the international cross-sectional and longitudinal assessment on asthma control (LIAISON) study. Respir Res 2016; 17(1): 51, https://doi.org/10.1186/s12931-016-0374-z.
- Veenendaal M., Westerik J.A.M., van den Bemt L., Kocks J.W.H., Bischoff E.W., Schermer T.R. Age- and sex-specific prevalence of chronic comorbidity in adult patients with asthma: a real-life study. NPJ Prim Care Respir Med 2019; 29(1): 14, https://doi.org/10.1038/s41533-019-0127-9.
- Majellano E.C., Clark V.L., Winter N.A., Gibson P.G., McDonald V.M. Approaches to the assessment of severe asthma: barriers and strategies. J Asthma Allergy 2019; 12: 235–251, https://doi.org/10.2147/JAA.S178927.
- Bousquet J.J., Schunemann H.J., Togias A., Erhola M., Hellings P.W., Zuberbier T., Agache I., Ansotegui I.J., Anto J.M., Bachert C., Becker S., Bedolla-Barajas M., Bewick M., Bosnic-Anticevich S., Bosse I., Boulet L.P., Bourrez J.M., Brusselle G., Chavannes N., Costa E., Cruz A.A., Czarlewski W., Fokkens W.J., Fonseca J.A., Gaga M., Haahtela T., Illario M., Klimek L., Kuna P., Kvedariene V., Le L.T.T., Larenas-Linnemann D., Laune D., Lourenco O.M., Menditto E., Mullol J., Okamoto Y., Papadopoulos N., Pham-Thi N., Picard R., Pinnock H., Roche N., Roller-Wirnsberger R.E., Rolland C., Samolinski B., Sheikh A., Toppila-Salmi S., Tsiligianni I., Valiulis A., Valovirta E., Vasankari T., Ventura M.T., Walker S., Williams S., Akdis C.A., Annesi-Maesano I., Arnavielhe S., Basagana X., Bateman E., Bedbrook A., Bennoor K.S., Benveniste S., Bergmann K.C., Bialek S., Billo N., Bindslev-Jensen C., Bjermer L., Blain H., Bonini M., Bonniaud P., Bouchard J., Briedis V., Brightling C.E., Brozek J., Buhl R., Buonaiuto R., Canonica G.W., Cardona V., Carriazo A.M., Carr W., Cartier C., Casale T., Cecchi L., Cepeda Sarabia A.M., Chkhartishvili E., Chu D.K., Cingi C., Colgan E., de Sousa J.C., Courbis A.L., Custovic A., Cvetkosvki B., D’Amato G., da Silva J., Dantas C., Dokic D., Dauvilliers Y., Dedeu A., De Feo G., Devillier P., Di Capua S., Dykewickz M., Dubakiene R., Ebisawa M., El-Gamal Y., Eller E., Emuzyte R., Farrell J., Fink-Wagner A., Fiocchi A., Fontaine J.F., Gemicioglu B., Schmid-Grendelmeir P., Gamkrelidze A., Garcia-Aymerich J., Gomez M., Gonzalez Diaz S., Gotua M., Guldemond N.A., Guzman M.A., Hajjam J., O’B Hourihane J., Humbert M., Iaccarino G., Ierodiakonou D., Ivancevich J.C., Joos G., Jung K.S., Jutel M., Kaidashev I., Kalayci O., Kardas P., Keil T., Khaitov M., Khaltaev N., Kleine-Tebbe J., Kowalski M.L., Kritikos V., Kull I., Leonardini L., Lieberman P., Lipworth B., Lodrup Carlsen K.C., Loureiro C.C., Louis R., Mair A., Marien G., Mahboub B., Malva J., Manning P., de Manuel Keenoy E., Marshall G.D., Masjedi M.R., Maspero J.F., Mathieu-Dupas E., Matricardi P.M., Melen E., Melo-Gomes E., Meltzer E.O., Mercier J., Miculinic N., Mihaltan F., Milenkovic B., Moda G., Mogica-Martinez M.D., Mohammad Y., Montefort S., Monti R., Morais-Almeida M., Mosges R., Munter L., Muraro A., Murray R., Naclerio R., Napoli L., Namazova-Baranova L., Neffen H., Nekam K., Neou A., Novellino E., Nyembue D., O’Hehir R., Ohta K., Okubo K., Onorato G., Ouedraogo S., Pali-Scholl I., Palkonen S., Panzner P., Park H.S., Pepin J.L., Pereira A.M., Pfaar O., Paulino E., Phillips J., Plavec D., Popov T.A., Portejoie F., Price D., Prokopakis E.P., Pugin B., Raciborski F., Rajabian-Soderlund R., Reitsma S., Rodo X., Romano A., Rosario N., Rottem M., Ryan D., Salimaki J., Sanchez-Borges M.M., Sisul J.C., Sole D., Somekh D., Sooronbaev T., Sova M., Spranger O., Stellato C., Stelmach R., Suppli Ulrik C., Thibaudon M., To T., Todo-Bom A., Tomazic P.V., Valero A.A., Valenta R., Valentin-Rostan M., van der Kleij R., Vandenplas O., Vezzani G., Viart F., Viegi G., Wallace D., Wagenmann M., Wang Y., Waserman S., Wickman M., Williams D.M., Wong G., Wroczynski P., Yiallouros P.K., Yorgancioglu A., Yusuf O.M., Zar H.J., Zeng S., Zernotti M., Zhang L., Zhong N.S., Zidarn M.; ARIA Study Group; MASK Study Group. Next-generation ARIA care pathways for rhinitis and asthma: a model for multimorbid chronic diseases. Clin Transl Allergy 2019; 9: 44, https://doi.org/10.1186/s13601-019-0279-2.
- Eliseeva T.I., Krasilnikova S.V., Babaev S.Y., Novozhilov A.A., Ovsyannikov D.Y., Ignatov S.K., Kubysheva N.I., Shakhov A.V. Dependence of anterior active rhinomanometry indices on nasal obstructive disorders in children with atopic bronchial asthma complicated by nasal symptoms. Biomed Res Int 2018: 1869613, https://doi.org/10.1155/2018/1869613.
- Eliseeva T.I., Krasilnikova S.V., Geppe N.A., Babaev S.Y., Tush E.V., Khaletskaya O.V., Ovsyannikov D.Y., Balabolkin I.I., Ignatov S.K., Kubysheva N.I. Effect of nasal obstructive disorders on sinonasal symptoms in children with different levels of bronchial asthma control. Can Respir J 2018: 4835823, https://doi.org/10.1155/2018/4835823.
- Jiang D., Wang L., Bai C., Chen O. Association between abdominal obesity and asthma: a meta-analysis. Allergy Asthma Clin Immunol 2019; 15: 16, https://doi.org/10.1186/s13223-019-0333-6.
- GINA. The Global Asthma Report 2018. Auckland, New Zealand: Global Asthma Network; 2018. URL: http://www.globalasthmareport.org/ Global%20Asthma%20Report%202018.pdf.
- World Health Organization. Obesity and overweight. 2020. URL: https://www.who.int/news-room/fact- sheets/detail/obesity-and-overweight.
- Salome C.M., King G.G., Berend N. Physiology of obesity and effects on lung function. J Appl Physiol (1985) 2010; 108(1): 206–211, https://doi.org/10.1152/japplphysiol.00694.2009.
- Yao T.C., Tsai H.J., Chang S.W., Chung R.H., Hsu J.Y., Tsai M.H., Liao S.L., Hua M.C., Lai S.H., Chen L.C., Yeh K.W., Tseng Y.L., Lin W.C., Chang S.C., Huang J.L.; Prediction of Allergies in Taiwanese Children (PATCH) Study Group. Obesity disproportionately impacts lung volumes, airflow and exhaled nitric oxide in children. PloS One 2017; 12(4): e0174691, https://doi.org/10.1371/journal.pone.0174691.
- Melo L.C., Silva M.A., Calles A.C. Obesity and lung function: a systematic review. Einstein (Sao Paulo) 2014; 12(1): 120–125, https://doi.org/10.1590/s1679-45082014rw2691.
- Pijnenburg M.W., Baraldi E., Brand P.L., Carlsen K.H., Eber E., Frischer T., Hedlin G., Kulkarni N., Lex C., Mäkelä M.J., Mantzouranis E., Moeller A., Pavord I., Piacentini G., Price D., Rottier B.L., Saglani S., Sly P.D., Szefler S.J., Tonia T., Turner S., Wooler E., Lødrup Carlsen K.C. Monitoring asthma in children. Eur Respir J 2015; 45(4): 906–925, https://doi.org/10.1183/09031936.00088814.
- Eliseeva Т.I., Knyazeva Е.V., Bochkova Y.S., Kononova S.V., Geppe N.A., Balabolkin I.I. Spirographic parameters and their change in bronchial patency variability tests in control level assessment of bronchial asthma in children. Sovremennye tehnologii v medicine 2013; 5(4): 94–101.
- Eliseeva Т.I., Knyazeva Е.V., Geppe N.A., Balabolkin I.I. The relationship of spirographic parameters and bronchial responsiveness with asthma control level in children (according to ACQ-5 and АСТ-С data). Sovremennye tehnologii v medicine 2013; 5(2): 47–52.
- Forno E., Celedón J.C. The effect of obesity, weight gain, and weight loss on asthma inception and control. Curr Opin Allergy Clin Immunol 2017; 17(2): 123–130, https://doi.org/10.1097/ACI.0000000000000339.
- Forno E., Han Y.Y., Mullen J., Celedón J.C. Overweight, obesity, and lung function in children and adults — a meta-analysis. J Allergy Clin Immunol Pract 2018; 6(2): 570–581.e10, https://doi.org/10.1016/j.jaip.2017.07.010.
- Kasteleyn M.J., Bonten T.N., de Mutsert R., Thijs W., Hiemstra P.S., le Cessie S., Rosendaal F.R., Chavannes N.H., Taube C. Pulmonary function, exhaled nitric oxide and symptoms in asthma patients with obesity: a cross-sectional study. Respir Res 2017; 18(1): 205, https://doi.org/10.1186/s12931-017-0684-9.
- Somashekar A.R., Sowmya A.N. Co-relation of body mass index with the prevalence and severity of asthma in urban children aged 7–12 years. J Pediatr Care 2016; 2: 2, https://doi.org/10.21767/2471-805X.100012.
- Wang R., Custovic A., Simpson A., Belgrave D.C., Lowe L.A., Murray C.S. Differing associations of BMI and body fat with asthma and lung function in children. Pediatr Pulmonol 2014; 49(11): 1049–1057, https://doi.org/10.1002/ppul.22927.
- Tantisira K.G., Litonjua A.A., Weiss S.T., Fuhlbrigge A.L. Association of body mass with pulmonary function in the Childhood Asthma Management Program (CAMP). Thorax 2003; 58(12): 1036–1041, https://doi.org/10.1136/thorax.58.12.1036.
- Eliseeva Т.I., Geppe N.A., Ignatov S.K., Soodaeva S.K., Tush Е.V., Khaletskaya O.V., Potemina T.E., Malakhov A.B., Kubysheva N.I., Solovyov V.D. Relative body mass index as a new tool for nutritional status assessment in children and adolescents with bronchial asthma. Sovremennye tehnologii v medicine 2017; 9(1): 135–148, https://doi.org/10.17691/stm2017.9.1.18.
- Pruszkowska-Przybylska P., Sitek A., Rosset I., Żądzińska E., Sobalska-Kwapis M., Słomka M., Strapagiel D. The association between socioeconomic status, duration of breastfeeding, parental age and birth parameters with BMI, body fat and muscle mass among prepubertal children in Poland. Anthropol Anz 2019; 76(5): 409–419, https://doi.org/10.1127/anthranz/2019/0955.
- Lele R.D. Fat and muscle component of body mass index (BMI): relation with hyperinsulinemia. J Assoc Physicians India 2007; 55: 203–210.
- Sutherland T.J., McLachlan C.R., Sears M.R., Poulton R., Hancox R.J. The relationship between body fat and respiratory function in young adults. Eur Respir J 2016; 48(3): 734–747, https://doi.org/10.1183/13993003.02216-2015.
- Kamal R., Kesavachandran C.N., Bihari V., Sathian B., Srivastava A.K. Alterations in lung functions based on BMI and body fat % among obese indian population at national capital region. Nepal J Epidemiol 2015; 5(2): 470–479, https://doi.org/10.3126/nje.v5i2.12829.
- Alaagib N., Sukkar M.Y. Effect of body composition on ventilation parameters in a group of young Sudanese females. Sudan Journal of Medical Sciences 2017; 12: 78, https://doi.org/10.18502/sjms.v12i2.918.
- McLachlan C.R., Poulton R., Car G., Cowan J., Filsell S., Greene J.M., Taylor D.R., Welch D., Williamson A., Sears M.R., Hancox R.J. Adiposity, asthma, and airway inflammation. J Allergy Clin Immunol 2007; 119(3): 634–639, https://doi.org/10.1016/j.jaci.2006.10.029.
- Myung J., Lee H., Kim T.H., Han E. Relationships between self-reported asthma and pulmonary function and various measures of obesity. J Asthma 2018; 55(7): 741–749, https://doi.org/10.1080/02770903.2017.1362701.
- Kongkiattikul L., Sritippayawan S., Chomtho S., Deerojanawong J., Prapphal N. Relationship between obesity indices and pulmonary function parameters in obese thai children and adolescents. Indian J Pediatr 2015; 82(12): 1112–1116, https://doi.org/10.1007/s12098-015-1777-4.
- Mukherjee S., Mukhopadhyay D.K. Association between body mass index (BMI), body fat percentage and pulmonary functions in obese, overweight and normal weight adolescents. Journal of Evolution of Medical and Dental Sciences 2018; 7(44): 5589–5593, https://doi.org/10.14260/jemds/2018/1068.
- GINA. Global strategy for asthma management and prevention. Global Initiative for Asthma (GINA); 2016.
- Ovsyannikov D.Y., Kuzmenko L.G., Nazarova T.I., Haled M., Frolov P.A., Nguen B.V., Illarionova T.Y., Semyatov S.M., Eliseeva T.I. Clinical and laboratory markers of bacterial infection in children of different ages. Pediatria 2019; 98(1): 186–192, https://doi.org/10.24110/0031-403X-2019-98-1-186-192.
- Nilova M.Y., Tush E.V., Eliseeva Т.I., Krasilnikova S.V., Khaletskaya О.V., Popov K.S., Novikova N.A. Structure of sensitization to aeroallergenes in children with atopic bronchial asthma. Allergologiya i immunologiya v pediatrii 2019; 2: 17–23.
- Natale V., Rajagopalan A. Worldwide variation in human growth and the World Health Organization growth standards: a systematic review. BMJ Open 2014; 4(1): e003735, https://doi.org/10.1136/bmjopen-2013-003735.
- Juniper E.F., Bousquet J., Abetz L., Bateman E.D.; GOAL Committee. Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the asthma control questionnaire. Respir Med 2006; 100(4): 616–621, https://doi.org/10.1016/j.rmed.2005.08.012.
- Miller M.R., Hankinson J., Brusasco V., Burgos F., Casaburi R., Coates A., Crapo R., Enright P., van der Grinten C.P., Gustafsson P., Jensen R., Johnson D.C., MacIntyre N., McKay R., Navajas D., Pedersen O.F., Pellegrino R., Viegi G., Wanger J.; ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J 2005; 26(2): 319–338, https://doi.org/10.1183/09031936.05.00034805.
- Wells J.C. Sexual dimorphism of body composition. Best Pract Res Clin Endocrinol Metab 2007; 21(3): 415–430, https://doi.org/10.1016/j.beem.2007.04.007.
- Duncan G.S.J., Gharbawi N.T., Viskaduraki M., Gaillard E.A., Beardsmore C.S. P90. How does BMI status influence spirometry and respiratory muscle strength in children? Thorax 2017; 72(Suppl 3): A132, https://doi.org/10.1136/thoraxjnl-2017-210983.232.
- Cvejoska-Cholakovska V., Kocova M., Velikj-Stefanovska V., Vlashki E. The association between asthma and obesity in children — inflammatory and mechanical factors. Open Access Maced J Med Sci 2019; 7(8): 1314–1319, https://doi.org/10.3889/oamjms.2019.310.
- Sood A., Shore S.A. Adiponectin, leptin, and resistin in asthma: basic mechanisms through population studies. J Allergy (Cairo) 2013; 2013: 785835, https://doi.org/10.1155/2013/785835.
- Webering S., Lunding L.P., Vock C., Schroder A., Gaede K.I., Herzmann C., Fehrenbach H., Wegmann M. The alpha-melanocyte-stimulating hormone acts as a local immune homeostasis factor in experimental allergic asthma. Clin Exp Allergy 2019; 49(7): 1026–1039, https://doi.org/10.1111/cea.13400.
- Sutherland E.R., Goleva E., Strand M., Beuther D.A., Leung D.Y. Body mass and glucocorticoid response in asthma. Am J Respir Crit Care Med 2008; 178(7): 682–687, https://doi.org/10.1164/rccm.200801-076OC.
- Xiong X.F., Fan L.L., Wu H.X., Zhu M., Cheng D.Y. Effects of tiotropium combined with theophylline on stable COPD patients of group B, D and its impact on small airway function: a randomized controlled trial. Adv Ther 2018; 35(12): 2201–2213, https://doi.org/10.1007/s12325-018-0831-9.
- Sin D.D., Man S.F. Impaired lung function and serum leptin in men and women with normal body weight: a population based study. Thorax 2003; 58(8): 695–698, https://doi.org/10.1136/thorax.58.8.695.
- Jones R.L., Nzekwu M.M. The effects of body mass index on lung volumes. Chest 2006; 130(3): 827–833, https://doi.org/10.1378/chest.130.3.827.
- Real F.G., Svanes C., Omenaas E.R., Anto J.M., Plana E., Janson C., Jarvis D., Zemp E., Wjst M., Leynaert B., Sunyer J. Menstrual irregularity and asthma and lung function. J Allergy Clin Immunol 2007; 120(3): 557–64, https://doi.org/10.1016/j.jaci.2007.04.041.
- Real F.G., Svanes C., Macsali F., Omenaas E.R. Hormonal factors and respiratory health in women — a review. Clin Respir J 2008; 2(Suppl 1): 111–119, https://doi.org/10.1111/j.1752-699X.2008.00093.x.
- Jensen M.E., Wood L.G., Gibson P.G. Obesity and childhood asthma — mechanisms and manifestations. Curr Opin Allergy Clin Immunol 2012; 12(2): 186–192, https://doi.org/10.1097/ACI.0b013e3283508df5.
- Forno E., Weiner D.J., Mullen J., Sawicki G., Kurland G., Han Y.Y., Cloutier M.M., Canino G., Weiss S.T., Litonjua A.A., Celedón J.C. Obesity and airway dysanapsis in children with and without asthma. Am J Respir Crit Care Med 2017; 195(3): 314–323, https://doi.org/10.1164/rccm.201605-1039OC.
- Han Y.Y., Forno E., Celedon J.C. Adiposity, fractional exhaled nitric oxide, and asthma in U.S. children. Am J Respir Crit Care Med 2014; 190(1): 32–39, https://doi.org/10.1164/rccm.201403-0565OC.
- Cibella F., Bruno A., Cuttitta G., Bucchieri S., Melis M.R., De Cantis S., La Grutta S., Viegi G. An elevated body mass index increases lung volume but reduces airflow in Italian schoolchildren. PloS One 2015; 10(5): e0127154, https://doi.org/10.1371/journal.pone.0127154.
- Spathopoulos D., Paraskakis E., Trypsianis G., Tsalkidis A., Arvanitidou V., Emporiadou M., Bouros D., Chatzimichael A. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol 2009; 44(3): 273–280, https://doi.org/10.1002/ppul.20995.
- Bekkers M.B., Wijga A.H., de Jongste J.C., Kerkhof M., Postma D., Gehring U., Smit H.A., Brunekreef B. Waist circumference, BMI, and lung function in 8-year-old children: the PIAMA birth cohort study. Pediatr Pulmonol 2013; 48(7): 674–82, https://doi.org/10.1002/ppul.22722.
- Davidson W.J., Mackenzie-Rife K.A., Witmans M.B., Montgomery M.D., Ball G.D., Egbogah S., Eves N.D. Obesity negatively impacts lung function in children and adolescents. Pediatr Pulmonol 2014; 49(10): 1003–1010, https://doi.org/10.1002/ppul.22915.
- Forbes L. Do exogenous oestrogens and progesterone influence asthma? Thorax 1999; 54(3): 265–267, https://doi.org/10.1136/thx.54.3.265.
- Varraso R., Siroux V., Maccario J., Pin I., Kauffmann F.; Epidemiological Study on the Genetics and Environment of Asthma. Asthma severity is associated with body mass index and early menarche in women. Am J Respir Crit Care Med 2005; 171(4): 334–339, https://doi.org/10.1164/rccm.200405-674OC.










