A Digital Electrocardiographic System for Assessing Myocardial Electrical Instability: Principles and Applications
The aim of the study was to develop an ECG hardware and software system for monitoring electrical instability of the myocardium and to assess the diagnostic and prognostic capabilities of this setup in a cardiology clinic.
Materials and Methods. The Intecard 7.3 software and hardware system developed in this study makes it possible to measure fluctuations of the ECG amplitude-time parameters using the beat-to-beat mode. Intecard 7.3 evaluates a number of ECG markers that reflect electrical instability of the myocardium. Among them are the fragmented QRS complex, the spatial QRS-T angle, the T-wave alternans, the duration, and dispersion of the QT interval, the turbulence and acceleration/deceleration of the heart rhythm.
Clinical trials of Intecard 7.3 were carried out with 734 patients with ischemic heart disease or cardiomyopathy and 112 healthy individuals.
Results. Intecard 7.3 reliably identifies fragmented QRS complexes by detecting short spikes of <25 ms in the ascending parts of the Q, R, and S waves. The QRS-T angle is determined from the reference amplitudes of the R and T waves in leads avF, V2, V5, and V6. Digital precision processing of the ECG signal improves its accuracy to microvolts and microseconds.
The software was designed to measure the T-wave amplitude in each of 300–500 cardiobeats; T-wave alternans was estimated by the moving average method. In a typical cardiobeat, the QT dispersion was calculated based on 12 ECG leads. From the sequence of RR intervals, turbulence, and deceleration of the heart rhythm were determined.
During the observation period of 5.0 [2.1; 5.9] years, 90 out of 734 patients (12.3%) experienced adverse cardiovascular events (ACVE). In this period, the myocardial electrical instability was recorded in patients with ACVE more frequently than in those without ACVE. Thus, the frequency of fragmented QRS was 72.2±4.7 vs 16.8±1.5% (p<0.01), the values of the QRS-T angle were 128 [55; 101] vs 80 [53; 121]° (p<0.001), the T-wave alternans — 36.9 [15.5; 62.1] vs 21.9 [10.2; 30.7] μV (p<0.005), the QT interval — 408 [383; 438] vs 376 [351; 400] ms (p<0.001), the QT dispersion — 76 [57; 96] vs 64 [50; 92] ms (p<0.005), respectively. In patients with ACVE, the threshold that triggers pathological rhythm turbulence was higher (>0%) than that in healthy controls (p<0.001); the deceleration of the heart rhythm was reduced from 19.2 [2.2; 38.0] to 8.8 [4.0; 16.8] ms (p<0.05).
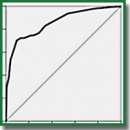
A personalized model for ACVE risk stratification has been developed. In this model, the area under the ROC curve was 0.856; sensitivity — 75%; specificity — 78%; predictive accuracy — 77%.
Conclusion. Using the ECG markers of myocardial electrical instability, the Intecard 7.3 system allows one to predict life-threatening ventricular tachyarrhythmias and sudden cardiac death with an accuracy of 77%. The non-invasiveness, high productivity, and reasonable cost ensure the availability of this predictive technology in all levels of healthcare.
- Sula A.S., Ryabykina G.V., Grishin V.G. ECG analyzer “Cardiovisor-06C”: new possibilities for detecting myocardial ischemia during screening examinations and prospects for use in functional diagnostics. Funkcionalnaya diagnostika 2003; 2: 64–77.
- Kolosova K.S., Grigoryeva N.Yu., Kosyuga Yu.I. High-frequency ECG for detection of myocardial ischemia associated with right coronary artery stenosis in IHD patients. Sovremennye tehnologii v medicine 2020; 12(1): 86–91, https://doi.org/10.17691/stm2020.12.1.11.
- Minina E.N., Faynzilberg L.S. Analysis of functional state of cardiovascular system by collection of the signs of phasic portrait in single channel ECG. Rossijskij kardiologiceskij zurnal 2015; 12: 7–13.
- Lampert R. ECG signatures of physiological stress. J Electrocardiol 2015; 48(6): 1000–1005, https://doi.org/10.1016/j.jelectrocard.2015.08.005.
- Pietrasik G., Zaręba W. QRS fragmentation: diagnostics and prognostic significance. Cardiol J 2012; 19(2): 114–121, https://doi.org/10.5603/cj.2012.0022.
- Kardys I., Kors J.A., van der Meer I.M., Hofman A., van der Kuip D.A., Witterman J.C. Spatial QRS-T angle predicts cardiac death in general population. Eur Heart J 2003; 24(14): 1357–1364, https://doi.org/10.1016/s0195-668x(03)00203-3.
- Verrier R.L., Klingenheben T., Malik M., El-Sherif N., Exner D.V., Hohnloser S.H., Ikeda T., Martínez J.P., Narayan S.M., Nieminen T., Rosenbaum D.S. Microvolt T-wave alternans. Physiological basic, methods of measurement, and clinical utility — consensus guideline by International Society for Holter and Noninvasive Electrocardiology. J Am Coll Cardiol 2011; 58(13): 1309–1324, https://doi.org/10.1016/j.jacc.2011.06.029.
- Malik M., Batchvarov V.N. Measurement, interpretation, and clinical potential of QT interval dispersion. J Am Coll Cardiol 2000; 36(6): 1749–1766, https://doi.org/10.1016/s0735-1097(00)00962-1.
- Bauer A., Malik M., Schmidt G., Barthel P., Bonnemeier H., Cygankiewicz I., Guzik P., Lombardi F., Müller A., Oto A., Schneider R., Watanabe M., Wichterle D., Zareba W. Heart rate turbulence: standards of measurement, physiological interpretation, and clinical use: International Society for Holter and Noninvasive Electrophysiology Consensus. J Am Coll Cardiol 2008; 52(17): 1353–1365, https://doi.org/10.1016/j.jacc.2008.07.041.
- Bauer A., Kantelhardt J.W., Barthel P., Schneider R., Mäkikallio T., Ulm K., Hnatkova K., Schömig A., Huikuri H., Bunde A., Malik M., Schmidt G. Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: cohort study. Lancet 2006; 367(9523): 1674–1681, https://doi.org/10.1016/s0140-6736(06)68735-7.
- Rautaharju P.M., Prineas R.J., Zhang Z.M. A simple procedure for estimation of the spatial QRS/T angle from the standard 12-lead electrocardiogram. J Electrocardiol 2007; 40(3): 300–304, https://doi.org/10.1016/j.jelectrocard.2006.11.003.
- Das M.K., Khan B., Jakob S., Kumar A., Mahenthiran J. Significance of fragmented QRS complex versus a Q wave in patients with coronary artery disease. Circulation 2006; 113(21): 2495–2501, https://doi.org/10.1161/circulationaha.105.595892.
- Sharma S., Jayakumar T., Rupesh G., Rajesh G., Chamanshaikh S.N., Deofi G., Abdulkhamar S. Significance of fragmented QRS complex in acute coronary syndrome and its correlation with coronary angiography to identify the culprit lesion. Int J Sci Stud 2016; 4(4): 246–252.
- Czub P., Cacko A., Gawałko M., Tataj E., Poliński J., Pawlik K., Cichoń R., Hendzel P. Perioperative risk assessment wih Euroscore and Euroscore II in patients with coronary artery and valvular desease. Medicine (Baltimore) 2018; 97(50): e13572, https://doi.org/10.1097/md.0000000000013572.










