Effect of Cryo-Processing on Platelet-Rich Autoplasma Preparations
Platelet-derived growth factor (PDGF) plays an important role in angiogenesis, affects activation of migration and proliferation of mesenchymal stem cells, fibroblasts, smooth muscle cells, osteoblasts; activation of migration of monocytes, macrophages, and neutrophils.
The aim of the investigation was to study the effect of cryo-processing on the qualitative properties of platelet-rich autoplasma (PRP) at different time intervals.
Materials and Methods. Autologous plasma preparations were obtained from the blood of 31 donors. The biological material was prepared by double centrifugation according to the protocol for obtaining P-PRP and L-PRP. Platelet count and the concentration of growth factors (PDGF-AA and PDGF-BB) were studied in fresh PRP preparations. In frozen PRP samples, the concentration of PDGF-AA and PDGF-BB was determined 2 weeks after cryo-processing and 2 months after cryo-processing at –35°С. P-PRP and L-PRP samples activated with 10% CaCl2 solution and those non-activated were studied.
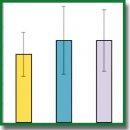
Results. L-PRP preparations are significantly superior to P-PRP preparations: the concentration of platelets is 1.7 times higher in them. The level of PDGF-AA in non-activated L-PRP is 1.8 times higher than in non-activated P-PRP (p<0.05). The level of PDGF-AA is 1.5 times higher in activated L-PRP than in activated P-PRP (p<0.05). The level of PDGF-BB is 2.9 times higher in non-activated L-PRP than in non-activated P-PRP and 1.8 times higher in activated L-PRP than in activated P-PRP (p<0.05). The concentration of PDGF-BB in non-activated P-PRP sharply increases in the 2nd week after freezing and remains at the same level after 2 months (p<0.05). The concentration of PDGF-BB in activated plasma does not change (p>0.05).
Conclusion. Cryo-processing of non-activated autologous L-PRP allows preserving and subsequently enhancing the properties of plasma concentrate, which makes it possible to apply it in clinical practice.
- Brown S.A., Levi B., Lequex C., Wong V.W., Mojallal A., Longaker M.T. Basic science review on adipose tissue for clinicians. Plast Reconstr Surg 2010; 126(6): 1936–1946, https://doi.org/10.1097/prs.0b013e3181f44790.
- Turner A., Abu-Ghname A., Davis M.J., Winocour S.J., Hanson S.E., Chu C.K. Fat grafting in breast reconstruction. Semin Plast Surg 2020; 34(1): 17–23, https://doi.org/10.1055/s-0039-1700959.
- Rigotti G., Marchi A., Galiè M., Baroni G., Benati D., Krampera M., Pasini A., Sbarbati A. Clinical treatment of radiotherapy tissue demage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 2007; 119(5): 1409–1422, https://doi.org/10.1097/01.prs.0000256047.47909.71.
- Locke M.B., de Chalain T.M. Current practice in autologous fat transplantation: suggested clinical guidelines based on a review of recent literature. Ann Plast Surg 2008; 60(1): 98–102, https://doi.org/10.1097/sap.0b013e318038f74c.
- Fernandes G., Yang S. Application of platelet-rich plasma with stem cells in bone and periodontal tissue engineering. Bone Res 2016; 4: 16036, https://doi.org/10.1038/boneres.2016.36.
- Kon E., Filardo G., Di Matteo B., Marcacci M. PRP for the treatment of cartilage pathology. Open Orthop J 2013; 7: 120–128, https://doi.org/10.2174/1874325001307010120.
- Gonshor A. Technique for producing platelet-rich plasma and platelet concentrate: background and process. Int J Periodontics Restorative Dent 2002; 22(6): 547–557.
- Marx R.E., Carlson E.R., Eichstaedt R.M., Schimmele S.R., Strauss J.E., Georgeff K.R. Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85(6): 638–646, https://doi.org/10.1016/s1079-2104(98)90029-4.
- Marx R.E. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 2001; 10(4): 225–228, https://doi.org/10.1097/00008505-200110000-00002.
- Jain N.K., Gulati M. Platelet-rich plasma: a healing virtuoso. Blood Res 2016; 51(1): 3–5, https://doi.org/10.5045/br.2016.51.1.3.
- Marx R.E. In situ tissue engineering bone regeneration in jaw reconstructiong. Transl Regen Med 2015; 31: 437–447, https://doi.org/10.1016/b978-0-12-410396-2.00031-1.
- Kevy S.V., Jacobson V.S. Comparison of methods for point of care preparation of autologous platelet gel. J Extra Corpr Technol 2004; 36(1): 28–35.
- Alves R., Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord 2018; 4(1): 18–24, https://doi.org/10.1159/000477353.
- Eppley B.L., Woodell J.E., Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg 2004; 114(6): 1502–1508, https://doi.org/10.1097/01.prs.0000138251.07040.51.
- Weibrich G., Kleis W.K., Kunz-Kostomanolakis M., Loos A.H., Wagner W. Correlation of platelet concentration in platelet-rich plasma to the extraction method, age, sex, and platelet count of the donor. Int J Oral Maxillofac Implants 2001; 16(5): 693–699.
- Issa J.P.M., Tiossi R., da Silva Mello A.S., Lopes R.A., Di Matteo M.A.S., Iyomasa M.M. PRP: a possibility in regenerative therapy. Int J Morphol 2007; 25(3): 587–590, https://doi.org/10.4067/s0717-95022007000300019.
- Sarban S., Tabur H., Baba F., Işıkan U.E. The positive impact of platelet-derived growth factor on the repair of full-thickness defects of articular cartilage. Eklem Hastalik Cerrahisi 2018; 30(2): 91–96, https://doi.org/10.5606/ehc.2019.64018.
- Samadi P., Sheykhhasan M., Khoshinani H.M. The use of platelet-rich plasma in aesthetic and regenerative medicine: a comprehensive review. Aesthetic Plast Surg 2019; 43(3): 803–814, https://doi.org/10.1007/s00266-018-1293-9.
- Masuki H., Okudera T., Watanebe T., Suzuki M., Nishiyama K., Okudera H., Nakata K., Uematsu K., Su C.Y., Kawase T. Growth factor and pro-inflammatory cytokine contents in platelet-rich plasma (PRP), plasma rich in growth factors (PRGF), advanced platelet-rich fibrin (A-PRF), and concentrated growth factors (CGF). Int J Implant Dent 2016; 2(1): 19, https://doi.org/10.1186/s40729-016-0052-4.
- Mazzocca A.D., McCarthy M.B.R., Chowaniec D.M., Cote M.P., Romeo A.A., Bradley J.P., Arciero R.A., Beitzel K. Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am 2012; 94(4): 308–316, https://doi.org/10.2106/jbjs.k.00430.
- Ehrenfest D.M., Bielecki T., Mishra A., Borzini P., Inchingolo F., Sammartino G., Rasmusson L., Everts P.A. In search of a consensus terminology in the field of platelet concentrates for surgical use: platelet-rich plasma (PRP), platelet-rich fibrin (PRF), fibrin gel polymerization and leukocytes. Curr Pharm Biotechnol 2012; 13(7): 1131–1137, https://doi.org/10.2174/138920112800624328.
- Zorina A.I., Zorin V.L., Cherkasov V.R. PRP in aesthetic medicine. Eksperimental’naya i klinicheskaya dermatokosmetologiya 2013; 6: 10–21.
- Mishra A., Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006; 34(11): 1774–1778, https://doi.org/10.1177/0363546506288850.
- Wasterlain A.S., Braun H.J., Dragoo J.L. Contents and formulations of platelet-rich plasma. Oper Tech Orthop 2012; 22(1): 33–42, https://doi.org/10.1053/j.oto.2011.11.001.
- Startseva O.I., Melnikov D.V., Zakharenko A.S., Kirillova K.A., Pishchikova E.D., Epifanova M.V., Safronov V.V., Istranov A.L. Method of augmentation mammoplasty. Patent RU 2675019. 2018.
- Andia I., Sánchez M., Maffulli N. Joint pathology and platelet-rich plasma therapies. Expert Opin Biol Ther 2012; 12(1): 7–22, https://doi.org/10.1517/14712598.2012.632765.
- Eppley B., Pietrzak W.S., Blanton M. Platelet-rich plasma: a review of biology and applications in plastic surgery. Plast Reconstr Surg 2006; 118(6): 147e–159e, https://doi.org/10.1097/01.prs.0000239606.92676.cf.
- Kazakos K., Lyras D.N., Verettas D., Tilkeridis K., Tryfonidis M. The use of autologous PRP gel as an aid in the management of acute trauma wounds. Injury 2009; 40(8): 801–805, https://doi.org/10.1016/j.injury.2008.05.002.
- Dohan D.M., Choukroun J., Diss A., Dohan S.L., Dohan A.J., Mouhyi J., Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101(3): e45–e50, https://doi.org/10.1016/j.tripleo.2005.07.009.
- Agrawal A.A. Evolution, current status and advances in application of platelet concentrate in periodontics and implantology. World J Clin Cases 2017; 5(5): 159–171, https://doi.org/10.12998/wjcc.v5.i5.159.










