Isolation of Circulating Tumor Cells from Peripheral Blood Samples of Cancer Patients Using Microfluidic Technology
The aim of the investigation was to study the potential of an innovative microfluidic technology for the isolation of circulating tumor cells (CTCs) from the peripheral blood samples of cancer patients.
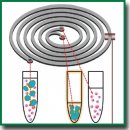
Materials and Methods. Peripheral blood samples from 5 patients with disseminated malignant tumors of epithelial origin were processedwith the use of the microfluidic technology (based on a specifically designed silicone chip). The cells were separated according to their density criterion based on the lateral migration of solid particles in a liquid due to inertial forces. With the help of the designed chip configuration, the cells over 13 μm in size which is larger than the standard size of blood cells were isolated. The resulting target cell fraction was stained by the Romanowsky–Giemsa method. Staining with the fluorescent Anti-Cytokeratin (CK3-6H5)-FITC antibody was carried out to confirm the epithelial nature of the cells, and the DAPI dye was used to contrast the nucleus. The blood of a healthy volunteer and tumor cells of the A549 line were used for the immunocytochemical studies.
Results. The tumor cells in peripheral blood (in the number of 1 to 9) were detected in all 5 patients. CTC clusters of 2–5 cells were identified in blood samples from the patients with laryngeal cancer, non-small cell lung cancer, and floor of the mouth cancer. A bright saturated staining of the A549 tumor cells was obtained using the Anti-Cytokeratin (CK3-6H5)-FITC antibody, corresponding to the staining of the cytoskeleton of epithelial cells. Successful nuclear staining with DAPI confirmed that the isolated target cells are not damaged during microfluidic separation.
Conclusion. The microfluidic technology that has been used enables effective intact CTCs isolating from the peripheral blood of cancer patients. The epithelial nature of the isolated cells can be confirmed by immunocytochemical studies.
- San Juan B.P., Garcia-Leon M.J., Rangel L., Goetz J.G., Chaffer C.L. The сomplexities of metastasis. Cancers (Basel) 2019; 11(10): 1575, https://doi.org/10.3390/cancers11101575.
- Chistiakov D.A., Chekhonin V.P. Circulating tumor cells and their advances to promote cancer metastasis and relapse, with focus on glioblastoma multiforme. Exp Mol Pathol 2018; 105(2): 166–174, https://doi.org/10.1016/j.yexmp.2018.07.007.
- Ashworth T.R. A case of cancer in which cells similar to those in the tumours were seen in the blood after death. Aust Med J 1869; 14: 146–149.
- Lugade A.A., Sorensen E.W., Gerber S.A., Moran J.P., Frelinger J.G., Lord E.M. Radiation-induced IFN-γ production within the tumor microenvironment influences antitumor immunity. J Immunol 2008; 180(5): 3132–3139, https://doi.org/10.4049/jimmunol.180.5.3132.
- Allard W.J., Matera J., Miller M.C., Repollet M., Connelly M.C., Rao C., Tibbe A.G., Uhr J.W., Terstappen L.W. Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res 2004; 10(20): 6897–6904, https://doi.org/10.1158/1078-0432.ccr-04-0378.
- McCorry A.M., Loughrey M.B., Longley D.B., Lawler M., Dunne P.D. Epithelial-to-mesenchymal transition signature assessment in colorectal cancer quantifies tumour stromal content rather than true transition. J Pathol 2018; 246(4): 422–426, https://doi.org/10.1002/path.5155.
- Saucedo-Zeni N., Mewes S., Niestroj R., Gasiorowski L., Murawa D., Nowaczyk P., Tomasi T., Weber E., Dworacki G., Morgenthaler N.G., Jansen H., Propping C., Sterzynska K., Dyszkiewicz W., Zabel M., Kiechle M., Reuning U., Schmitt M., Lücke K. A novel method for the in vivo isolation of circulating tumor cells from peripheral blood of cancer patients using a functionalized and structured medical wire. Int J Oncol 2012; 41(4): 1241–1250, https://doi.org/10.3892/ijo.2012.1557.
- Saliba A.E., Saias L., Psychari E., Minc N., Simon D., Bidard F.C., Mathiot C., Pierga J.Y., Fraisier V., Salamero J., Saada V., Farace F., Vielh P., Malaquin L., Viovy J.L. Microfluidic sorting and multimodal typing of cancer cells in self-assembled magnetic arrays. Proc Natl Acad Sci U S A 2010; 107(33): 14524–14529, https://doi.org/10.1073/pnas.1001515107.
- Bu J., Kang Y.T., Kim Y.J., Cho Y.H., Chang H.J., Kim H., Moon B.I., Kim H.G. Dual-patterned immunofiltration (DIF) device for the rapid efficient negative selection of heterogeneous circulating tumor cells. Lab Chip 2016; 16(24): 4759–4769, https://doi.org/10.1039/c6lc01179a.
- Buscail E., Alix-Panabières C., Quincy P., Cauvin T., Chauvet A., Degrandi O., Caumont C., Verdon S., Lamrissi I., Moranvillier I., Buscail C., Marty M., Laurent C., Vendrely V., Moreau-Gaudry F., Bedel A., Dabernat S., Chiche L. High clinical value of liquid biopsy to detect circulating tumor cells and tumor exosomes in pancreatic ductal adenocarcinoma patients eligible for up-front surgery. Cancers (Basel) 2019; 11(11): 1656, https://doi.org/10.3390/cancers11111656.
- Wu C., Hao H., Li L., Zhou X., Guo Z., Zhang L., Zhang X., Zhong W., Guo H., Bremner R.M., Lin P. Preliminary investigation of the clinical significance of detecting circulating tumor cells enriched from lung cancer patients. J Thorac Oncol 2009; 4(1): 30–36, https://doi.org/10.1097/jto.0b013e3181914125.
- Basu S., Campbell H.M., Dittel B.N., Ray A. Purification of specific cell population by fluorescence activated cell sorting (FACS). J Vis Exp 2010; 41: 1546, https://doi.org/10.3791/1546.
- Dalerba P., Kalisky T., Sahoo D., Rajendran P.S., Rothenberg M.E., Leyrat A.A., Sim S., Okamoto J., Johnston D.M., Qian D., Zabala M., Bueno J., Neff N.F., Wang J., Shelton A.A., Visser B., Hisamori S., Shimono Y., van de Wetering M., Clevers H., Clarke M.F., Quake S.R. Single-cell dissection of transcriptional heterogeneity in human colon tumors. Nat Biotechnol 2011; 29(12): 1120–1127, https://doi.org/10.1038/nbt.2038.
- Perfetto S.P., Chattopadhyay P.K., Roederer M. Seventeen-colour flow cytometry: unravelling the immune system. Nat Rev Immunol 2004; 4(8): 648–655, https://doi.org/10.1038/nri1416.
- Wang X., Sun L., Zhang H., Wei L., Qu W., Zeng Z., Liu Y., Zhu Z. Microfluidic chip combined with magnetic-activated cell sorting technology for tumor antigen-independent sorting of circulating hepatocellular carcinoma cells. Peer J 2019; 7: e6681, https://doi.org/10.7717/peerj.6681.
- Hofman V., Bonnetaud C., Ilie M.I., Vielh P., Vignaud J.M., Fléjou J.F., Lantuejoul S., Piaton E., Mourad N., Butori C., Selva E., Poudenx M., Sibon S., Kelhef S., Vénissac N., Jais J.P., Mouroux J., Molina T.J., Hofman P. Preoperative circulating tumor cell detection using the isolation by size of epithelial tumor cell method for patients with lung cancer is a new prognostic biomarker. Clin Cancer Res 2011; 17(4): 827–835, https://doi.org/10.1158/1078-0432.ccr-10-0445.
- Hosokawa M., Yoshikawa T., Negishi R., Yoshino T., Koh Y., Kenmotsu H., Naito T., Takahashi T., Yamamoto N., Kikuhara Y., Kanbara H., Tanaka T., Yamaguchi K., Matsunaga T. Microcavity array system for size-based enrichment of circulating tumor cells from the blood of patients with small-cell lung cancer. Anal Chem 2013; 85(12): 5692–5698, https://doi.org/10.1021/ac400167x.
- Gertler R., Rosenberg R., Fuehrer K., Dahm M., Nekarda H., Siewert J.R. Detection of circulating tumor cells in blood using an optimized density gradient centrifugation. Recent Results Cancer Res 2003; 162: 149–155, https://doi.org/10.1007/978-3-642-59349-9_13.
- Huang Q., Wang F.B., Yuan C.H., He Z., Rao L., Cai B., Chen B., Jiang S., Li Z., Chen J., Liu W., Guo F., Ao Z., Chen S., Zhao X.Z. Gelatin nanoparticle-coated silicon beads for density-selective capture and release of heterogeneous circulating tumor cells with high purity. Theranostics 2018; 8(6): 1624–1635, https://doi.org/10.7150/thno.23531.
- Segré G., Silberberg A. Radial particle displacements in Poiseuille flow of suspensions. Nature 1961; 189: 209–210.
- Segré G., Silberberg A. Behaviour of macroscopic rigid spheres in Poiseuille flow. Part 2. Experimental results and interpretation. J Fluid Mech 1962; 14(1): 136–157, https://doi.org/10.1017/S0022112062001111.
- Warkiani M.E., Khoo B.L., Wu L., Tay A.K., Bhagat A.A., Han J., Lim C.T. Ultra-fast, label-free isolation of circulating tumor cells from blood using spiral microfluidics. Nat Protoc 2016; 11(1): 134–148, https://doi.org/10.1038/nprot.2016.003.
- Lee P., Gaige T., Hung P. Microfluidic systems for live cell imaging. Methods Cell Biol 2011; 102: 77–103, https://doi.org/10.1016/b978-0-12-374912-3.00004-3.
- Valencia P.M., Farokhzad O.C., Karnik R., Langer R. Microfluidic technologies for accelerating the clinical translation of nanoparticles. Nat Nanotechnol 2012; 7(10): 623–629, https://doi.org/10.1038/nnano.2012.168.
- Deng Y., Zhang Y., Sun S., Wang Z., Wang M., Yu B., Czajkowsky D.M., Liu B., Li Y., Wei W., Shi Q. An integrated microfluidic chip system for single-cell secretion profiling of rare circulating tumor cells. Sci Rep 2014; 4: 7499, https://doi.org/10.1038/srep07499.
- Warkiani M.E., Guan G., Luan K.B., Lee W.C., Bhagat A.A., Chaudhuri P.K., Tan D.S., Lim W.T., Lee S.C., Chen P.C., Lim C.T., Han J. Slanted spiral microfluidics for the ultra-fast, label-free isolation of circulating tumor cells. Lab Chip 2014; 14(1): 128–137, https://doi.org/10.1039/c3lc50617g.
- Chaudhuri P.K., Ebrahimi Warkiani M., Jing T., Kenry, Lim C.T. Microfluidics for research and applications in oncology. Analyst 2016; 141(2): 504–524, https://doi.org/10.1039/c5an00382b.
- Shirani E., Razmjou A., Tavassoli H., Landarani-Isfahani A., Rezaei S., Abbasi Kajani A., Asadnia M., Hou J., Ebrahimi Warkiani M. Strategically designing a pumpless microfluidic device on an “inert” polypropylene substrate with potential application in biosensing and diagnostics. Langmuir 2017; 33(22): 5565–5576, https://doi.org/10.1021/acs.langmuir.7b00537.
- Freshni R.Ya. Kul’tura zhivotnykh kletok. Prakticheckoe rukovodstvo [Animal cell culture. A practical guide]. Moscow: BINOM. Laboratoriya znaniy; 2010; 714 p.










