Experience of Using Transpedicular Osteosynthesis in Traumatic Spondylolisthesis of the Axis
The aim of the study was to assess the efficacy and safety of direct posterior transpedicular osteosynthesis in traumatic spondylolisthesis of C2 vertebra.
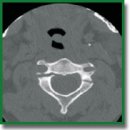
Materials and Methods. The present study is an observational retrospective analysis of the results of surgical treatment of 19 patients operated on in 2014–2020 using the posterior transpedicular osteosynthesis technique with Herbert’s compression screws for a Hangman’s fracture type II according to Levine–Edwards classification. After the operation, the follow-up period lasted for 22 [10; 36] months.
Results. The study group of patients (n=19) made 2.48% of all patients operated on for traumatic injury of the cervical spine (n=766) in the period from 2014 to 2020. In all cases, the surgical treatment was successful; there were no intraoperative complications in the form of damage to the vascular and nerve structures. The average duration of surgery was 70.8±24.5 min, and intraoperative blood loss was 92.9±41.8 ml. The length of hospitalization stay was 7 [5; 17] days. On the postoperative CT scans, no significant screw malposition (>2 mm) was found.
Conclusion. Transpedicular osteosynthesis with compression screws in C2 traumatic spondylolisthesis is a safe and sparing operation with a short duration and insignificant blood loss. Thorough preoperative planning and knowledge of the anatomic landmarks make it possible to perform this operation effectively under the C-arm X-ray system control without any navigation system.
- Anderson L.D., D’Alonzo R.T. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974; 56(8): 1663–1674.
- Robinson A.L., Olerud C., Robinson Y. Epidemiology of C2 fractures in the 21st century: a National Registry cohort study of 6,370 patients from 1997 to 2014. Adv Orthop 2017; 2017: 6516893, https://doi.org/10.1155/2017/6516893.
- Ryan M.D., Taylor T.K.F. Odontoid fractures in the elderly. J Spinal Disord 1993; 6(5): 397–401, https://doi.org/10.1097/00002517-199306050-00005.
- Vieweg U., Meyer B., Schramm J. Differential treatment in acute upper cervical spine injuries: a critical review of a single-institution series. Surg Neurol 2000; 54(3): 203–211, https://doi.org/10.1016/s0090-3019(00)00301-3.
- Benzel E.C., Hart B.L., Ball P.A., Baldwin N.G., Orrison W.W., Espinosa M. Fractures of the C-2 vertebral body. J Neurosurg 1994; 81(2): 206–212, https://doi.org/10.3171/jns.1994.81.2.0206.
- Hadley M.N., Dickman C.A., Browner C.M., Sonntag V.K. Acute axis fractures: a review of 229 cases. J Neurosurg 1989; 71(5 Pt 1): 642–647, https://doi.org/10.3171/jns.1989.71.5.0642.
- Schneider R.C., Livingston K.E., Cave A.J., Hamilton G. “Hangman’s fracture” of the cervical spine. J Neurosurg 1965; 22: 141–154, https://doi.org/10.3171/jns.1965.22.2.0141.
- Li X.F., Dai L.Y., Lu H., Chen X.D. A systematic review of the management of hangman’s fractures. Eur Spine J 2006; 15(3): 257–269, https://doi.org/10.1007/s00586-005-0918-2.
- Coric D., Wilson J.A., Kelly D.L. Jr. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg 1996; 85(4): 550–554, https://doi.org/10.3171/jns.1996.85.4.0550.
- Vaccaro A.R., Madigan L., Bauerle W.B., Blescia A., Cotler J.M. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976) 2002; 27(20): 2229–2233, https://doi.org/10.1097/00007632-200210150-00009.
- Ferro F.P., Borgo G.D., Letaif O.B., Cristante A.F., Marcon R.M., Lutaka A.S. Traumatic spondylolisthesis of the axis: epidemiology, management and outcome. Acta Ortop Bras 2012; 20(2): 84–87, https://doi.org/10.1590/s1413-78522012000200005.
- Al-Mahfoudh R., Beagrie C., Woolley E., Zakaria R., Radon M., Clark S., Pillay R., Wilby M. Management of typical and atypical hangman’s fractures. Global Spine J 2016; 6(3): 248–256, https://doi.org/10.1055/s-0035-1563404.
- Prost S., Barrey C., Blondel B., Fuentes S., Barresi L., Nicot B., Challier V., Lleu M., Godard J., Kouyoumdjian P., Lonjon N., Marinho P., Freitas E., Schuller S., Allia J., Berthiller J., Charles Y.P.; French Society for Spine Surgery (SFCR). Hangman’s fracture: management strategy and healing rate in a prospective multi-centre observational study of 34 patients. Orthop Traumatol Surg Res 2019; 105(4): 703–707, https://doi.org/10.1016/j.otsr.2019.03.009.
- Bazhanov S.P., Gulyaev D.A., Norkin I.A., Ostrovskiy V.V., Primak N.A. Method for posterior spinal fusion in traumatic injuries of upper cervical spine. Patent RU 2511485. 2014.
- Leconte P. Fracture et luxation des deux premieres vertèbres cervicales. In: Luxation Congénitale de la Hanche. Fractures du Cou-de-pied Rachis Cervical. Actualités de Chirurgie Orthopédique de l’Hôpital Raymond-Poincaré, Vol 3. Judet R. (editor). Paris: Masson et Cie; 1964; p. 147–166.
- Judet R., Roy-Camille R., Saillant G. Actualités de chirurgie orthopédique de l’Hospital Raymond-Poincaré. In: Judet R. (editor). Fractures du rachis cervical. Paris: Masson; 1970; p. 174–195.
- Levine A.M., Edwards C.C. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985; 67(2): 217–226.
- Effendi B., Roy D., Cornish B., Dussault R.G., Laurin C.A. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br 1981; 63-B(3): 319–327, https://doi.org/10.1302/0301-620x.63b3.7263741.
- Ma W., Xu R., Liu J., Sun S., Zhao L., Hu Y., Jiang W., Liu G., Gu Y. Posterior short-segment fixation and fusion in unstable hangman’s fractures. Spine (Phila Pa 1976) 2011; 36(7): 529–533, https://doi.org/10.1097/brs.0b013e3181d60067.
- Xie N., Khoo L.T., Yuan W., Ye X.J., Chen D.Y., Xiao J.R., Ni B. Combined anterior C2–C3 fusion and C2 pedicle screw fixation for the treatment of unstable hangman’s fracture: a contrast to anterior approach only. Spine (Phila Pa 1976) 2010; 35(6): 613–619, https://doi.org/10.1097/brs.0b013e3181ba3368.
- Ying Z., Wen Y., Xinwei W., Yong T., Hongyu L., Zhu H., Qinggang Z., Weihong Z., Yonggeng C. Anterior cervical discectomy and fusion for unstable traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976) 2008; 33(3): 255–258, https://doi.org/10.1097/brs.0b013e31816233d0.
- Gubin A.V., Burtsev A.V., Ryabikh S.O. Posterior fixation of hangman’s fractures. Hirurgia pozvonocnika 2014; 4: 15–19, https://doi.org/10.14531/ss2014.4.15-19.
- ElMiligui Y., Koptan W., Emran I. Transpedicular screw fixation for type II hangman’s fracture: a motion preserving procedure. Eur Spine J 2010; 19(8): 1299–1305, https://doi.org/10.1007/s00586-010-1401-2.
- Borne G.M., Bedou G.L., Pinaudeau M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg 1984; 60(1): 88–93, https://doi.org/10.3171/jns.1984.60.1.0088.
- Verheggen R., Jansen J. Hangman’s fracture: arguments in favor of surgical therapy for type II and III according to Edwards and Levine. Surg Neurol 1998; 49(3): 253–262, https://doi.org/10.1016/s0090-3019(97)00300-5.
- Boullosa J.L., Colli B.O., Carlotti C.G. Jr., Tanaka K., dos Santos M.B. Surgical management of axis’ traumatic spondylolisthesis (hangman’s fracture). Arq Neuropsiquiatr 2004; 62(3B): 821–826, https://doi.org/10.1590/s0004-282x2004000500015.
- Hakało J., Wroński J. Operative treatment of hangman’s fractures of C2. Posterior direct pars screw repair or anterior plate-cage stabilization? Neurol Neurochir Pol 2008; 42(1): 28–36.
- Liu Y., Zhu Y., Li X., Chen J., Yang S., Yang H., Jiang W. A new transpedicular lag screw fixation for treatment of unstable Hangman’s fracture: a minimum 2-year follow-up study. J Orthop Surg Res 2020; 15(1): 372, https://doi.org/10.1186/s13018-020-01911-3.
- Ludwig S.C., Kowalski J.M., Edwards C.C. 2nd, Heller J.G. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine (Phila Pa 1976) 2000; 25(20): 2675–2681, https://doi.org/10.1097/00007632-200010150-00022.
- Abumi K., Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997; 22(16): 1853–1863, https://doi.org/10.1097/00007632-199708150-00010.










