Surgical Treatment of Intramedullary Hemangioblastomas: Current State of Problem (Review)
Intramedullary hemangioblastomas (HAB) refer to very rare highly vascularized vascular spinal cord tumors associated with various neurological disorders. Effective HAB therapy to a greater extent depends on diagnostic accuracy and the absence of intra- and postoperative complications.
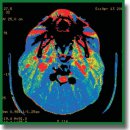
The present study is a review of publications concerned with modern diagnostic and therapeutic techniques to control spinal HAB. The authors showed that perfusion computed tomography, computed tomographic angiography, and magnetic resonance angiography can be reasonably used for diagnosis and differentiation in a number of HAB due to their high vascularization. Preoperative embolization significantly reducing intraoperative bleeding risks is highly efficient. Some authors recommend this procedure in case of large lesions and high risks of intraoperative bleeding. The review also considered intraoperative imaging of a tumor and its feeding vessels using indocyanine green providing inspectability over the total tumor resection and clear imaging of tumor vascular architecture. The advantages and restrictions of the mentioned procedures were described.
- Bamps S., Calenbergh F.V., Vleeschouwer S.D., Loon J.V., Sciot R., Legius E., Goffin J. What the neurosurgeon should know about hemangioblastoma, both sporadic and in von Hippel–Lindau disease: a literature review. Surg Neurol Int 2013; 4: 145, https://doi.org/10.4103/2152-7806.121110.
- Sun H.I., Ozduman K., Usseli M.I., Ozgen S., Pamir M.N. Sporadic spinal hemangioblastomas can be effectively treated by microsurgery alone. World Neurosurg 2014; 82(5): 836–847, https://doi.org/10.1016/j.wneu.2014.05.024.
- Samartzis D., Gillis C.C., Shih P., O’Toole J.E., Fessler R.G. Intramedullary spinal cord tumors: part I — epidemiology, pathophysiology, and diagnosis. Global Spine J 2015; 5(5): 425–435, https://doi.org/10.1055/s-0035-1549029.
- Metelo A., Iliopoulos O. Hemangioblastomas of the central nervous system. In: Rosenberg’s molecular and genetic basis of neurological and psychiatric disease. Academic Press; 2015; p. 955–961.
- Neumann H.P., Eggert H.R., Weigel K., Friedburg H., Wiestler O.D., Schollmeyer P. Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel–Lindau syndrome. J Neurosurg 1989; 70(1): 24–30, https://doi.org/10.3171/jns.1989.70.1.0024.
- Westwick H.J., Giguere J.F., Shamji M.F. Incidence and prognosis of spinal hemangioblastoma: a surveillance epidemiology and end results study. Neuroepidemiol 2015; 46(1): 14–23, https://doi.org/10.1159/000441147.
- Chamberlain M.C., Tredway T.L. Adult primary intradural spinal cord tumors: a review. Curr Neurol Neurosci Rep 2011; 11(3): 320–328, https://doi.org/10.1007/s11910-011-0190-2.
- Raco A., Esposito V., Lenzi J., Piccirilli M., Delfini R., Cantore G. Long-term follow-up of intramedullary spinal cord tumors: a series of 202 cases. Neurosurg 2005; 56(5): 972–981.
- Khan N.R., Ghazanfar A., Patel N., Arnautovic K.I. Spinal cord hemangioblastomas. In: Spinal cord tumors. Arnautovic K.I., Gokaslan Z.L. (editors). Springer, Cham; 2019; p. 243–271.
- Savintseva Zh.I., Trofimova T.N., Prakhova L.N., Nazinkina Yu.V., Skvortsova T.Yu. Diagnostics of intramedullary spinal cord tumors. Lucevaa diagnostika i terapia 2014; 2: 46–56.
- Takemoto K., Matsumura Y., Hashimoto H., Inoue Y., Fukuda T., Shakudo M., Nemoto Y., Onoyama Y., Yasui T., Hakuba A., Nishimura S., Ban S. MR imaging of intraspinal tumors — capability in histological differentiation and compartmentalization of extramedullary tumors. Neuroradiology 1988; 30(4): 303–309, https://doi.org/10.1007/bf00328180.
- Lee M., Epstein F.J., Rezai A.R., Zagzag D. Nonneoplastic intramedullary spinal cord lesions mimicking tumors. Neurosurgery 1998; 43(4): 788–795, https://doi.org/10.1097/00006123-199810000-00034.
- Parizel P.M., Baleriaux D., Rodesch G., Segebarth C., Lalmand B., Christophe C., Lemort M., Haesendonck P., Niendorf H.P., Flament-Durand J., Brotchi J. Gd-DTPA enhanced MR imaging of spinal tumors. AJR Am J Roentgenol 1989; 152(5): 1087–1096, https://doi.org/10.2214/ajr.152.5.1087.
- Froment J.C., Baleriaux D., Turjman F. Diagnosis: neuroradiology. In: Intramedullary spinal cord tumors. Fischer G., Brotchi J. (editors). Stuttgart: Thieme; 1996; p. 33–52.
- Bublievsky D.V., Evzikov G.Yu., Farafontov A.V., Shashkova E.V. Clinical signs, diagnostics and surgical treatment results at patients with spinal hemangioblastomas. Neirokhirurgiya 2013; 3: 15–23.
- Osborn A.G. Tumors, cysts, and tumorlike lesions of the spine and spinal cord. In: Diagnostic neuroradiology. St. Louis: Mosby Year Book; 1994; p. 895–916.
- Baleriaux D., Parizel P., Bank W.O. Intraspinal and intramedullary pathology. In: Imaging of the spine and spinal cord. Menelfe C. (editor). New York: Raven Press; 1992; p. 832–890.
- Na J.H., Kim H.S., Eoh W., Kim J.H., Kim J.S., Kim E.S. Spinal cord hemangioblastoma: diagnosis and clinical outcome after surgical treatment. J Korean Neurosurg Soc 2007; 42(6): 436–440, https://doi.org/10.3340/jkns.2007.42.6.436.
- Merhemic Z., Thurnher M.M. Diagnostics and differential diagnostics of spinal cord tumors. In: Spinal cord tumors. Arnautovic K.I., Gokaslan Z.L. (editors). Springer, Cham; 2019; p. 55–70.
- Dolgushin M. Kornienko V., Pronin I. Hemangioblastoma. In: Brain methastases. Springer, Cham; 2018; p. 375–376, https://doi.org/10.1007/978-3-319-57760-9_33.
- Leonov M.A., Arutyunov N.V., Kornienko V.N. X-ray diagnosis of hemangioblastomas of the posterior cranial fossa. Voprosy neirokhirurgii im. N.N. Burdenko 2005; 1: 20–23.
- Anderson I., Kumar R., Patankar T., Tyagi A. Lateral ventricle haemangioblastoma: the role of perfusion scanning and embolisation in diagnosis and management. BMJ Case Rep 2014: bcr2014205736, https://doi.org/10.1136/bcr-2014-205736.
- Clinical recommendations. Diagnostics and treatment of intramedullar spinal cord tumors. URL: https://ruans.org/Text/Guidelines/spinal_ intramedullary_tumors.pdf.
- Chen J.Q., Guan Y., Li G., Chen J.Q., Guan Y., Li G., Li X.H., Zhan Y.F., Li X.Y., Nie L., Han X.J. Application of 3D-computed tomography angiography technology in large meningioma resection. Asian Pac J Trop Med 2012; 5(7): 577–581, https://doi.org/10.1016/s1995-7645(12)60102-3.
- Matsumoto M., Kodama N., Endo Y., Sakuma J., Suzuki K., Sasaki T., Murakami K., Suzuki K., Katakura T., Shishido F. Dynamic 3D-CT angiography. AJNR Am J Neuroradiol 2007; 28(2): 299–304.
- Deng X., Wang K., Wu L., Yang C., Yang T., Zhao L., Yang J., Wang G., Fang J., Xu Y. Intraspinal hemangioblastomas: analysis of 92 cases in a single institution: clinical article. J Neurosurg Spine 2014; 21(2): 260–269, https://doi.org/10.3171/2014.1.spine13866.
- Seeger J.F., Burke D.P., Knake J.E., Gabrielsen T.O. Computed tomographic and angiographic evaluation of hemangioblastomas. Radiology 1981; 138(1): 65–73, https://doi.org/10.1148/radiology.138.1.7192875.
- Sciubba D.M., Mavinkurve G.G., Gailloud P., Garonzik I.M., Recinos P.F., McGirt M.J., Woodworth G.F., Witham T., Khavkin Y., Gokaslan Z.L., Wolinsky J.P. Preoperative imaging of cervical spine hemangioblastomas using three-dimensional fusion digital subtraction angiography. J Neurosurg Spine 2006; 5(1): 96–100, https://doi.org/10.3171/spi.2006.5.1.96.
- Yoshino M., Nakatomi H., Kin T., Saito T., Shono N., Nomura S., Nakagawa D., Takayanagi S., Imai H., Oyama H., Saito N. Usefulness of high-resolution 3D multifusion medical imaging for preoperative planning in patients with posterior fossa hemangioblastoma: technical note. J Neurosurg 2016; 127(1): 139–147, https://doi.org/10.3171/2016.5.jns152646.
- Abramova N.N., Belichenko O.I. Magnetic resonance tomography an magnetic resonance angiography in a visualization of vascular structures. Vestnik rentgenologii i radiologii 1997; 2: 50–54.
- Mascalchi M., Quilici N., Ferrito G., Mangiafico S., Scazzeri F., Torselli P., Petruzzi P., Cosottini M., Tessa С., Bartolozzi С. Identification of the feeding arteries of spinal vascular lesions via phase-contrast MR angiography with three-dimensional acquisition and phase display. AJNR Am J Neuroradiol 1997; 18(2): 351–358.
- Binkert C.A., Kollias S.S., Valavanis A. Spinal cord vascular disease: characterization with fast three-dimensional contrast-enhanced MR angiography. AJNR Am J Neuroradiol 1999; 20(10): 1785–1793.
- Crisi G., Giombelli E., Ventura E. Non-von Hippel–Lindau hemangioblastoma in the hippocampus: characterization with time-resolved MRA using TRICKS sequence at 3T. Neuroradiol J 2010; 23(4): 416–419, https://doi.org/10.1177/197140091002300407.
- Sayyahmelli S., Aycan A., Erginoglu U., Baskaya M.K. Spinal hemangioblastomas: clinical presentation, radiology, and treatment. Contemp Neurosurg 2019; 41(9): 1–5.
- Mehta G.U., Asthagiri A.R., Bakhtian K.D., Auh S., Oldfield E.H., Lonser R.R. Functional outcome after resection of spinal cord hemangioblastomas associated with von Hippel–Lindau disease. J Neurosurg Spine 2010; 12(3): 233–242, https://doi.org/10.3171/2009.10.spine09592.
- Harati A., Satopaa J., Mahler L., Billon-Grand R., Elsharkawy A., Niemela M., Hernesniemi J. Early microsurgical treatment for spinal hemangioblastomas improves outcome in patients with von Hippel–Lindau disease. Surg Neurol Int 2012; 3: 6, https://doi.org/10.4103/2152-7806.92170.
- Joaquim A.F., Ghizoni E., dos Santos M.J., Valadares M.G., da Silva F.S., Tedeschi H. Intramedullary hemangioblastomas: surgical results in 16 patients. Neurosurg Focus FOC 2015; 39(2): E18, https://doi.org/10.3171/2015.5.focus15171.
- Liu A., Jain A., Sankey E.W., Jallo G.I., Bettegowda C. Sporadic intramedullary hemangioblastoma of the spine: a single institutional review of 21 cases. Neurol Res
- 2016; 38(3): 205–209, https://doi.org/10.1179/1743132815y.0000000097.
- Das J.M., Kesavapisharady K., Sadasivam S., Nair S.N. Microsurgical treatment of sporadic and von Hippel–Lindau disease associated spinal hemangioblastomas: a single-institution experience. Asian Spine J 2017; 11(4): 548–555, https://doi.org/10.4184/asj.2017.11.4.548.
- Siller S., Szelenyi A., Herlitz L., Tonn J.C., Zausinger S. Spinal cord hemangioblastomas: significance of intraoperative neurophysiological monitoring for resection and long-term outcome. J Neurosurg Spine 2019; 26(4): 483–493, https://doi.org/10.3171/2016.8.spine16595.
- Chang H., Li J., Wang P., Lu X., Li B. Microsurgical treatment of cervical spinal hemangioblastoma. Neurochirurgie 2020; 66(1): 56–60, https://doi.org/10.1016/j.neuchi.2019.11.005.
- Wang H., Zhang L., Wang H., Nan Y., Ma Q. Spinal hemangioblastoma: surgical procedures, outcomes and review of the literature. Acta Neurol Belg 2021; 121(4): 973–981, https://doi.org/10.1007/s13760-020-01420-4.
- Parker F., Aghakhani N., Ducati L.G., Yacubian-Fernandes A., Silva M.V., David P., Richard S., Tadie M. Results of microsurgical treatment of medulla oblongata and spinal cord hemangioblastomas: a comparison of two distinct clinical patient groups. J Neurooncol 2009; 93(1): 133–137, https://doi.org/10.1007/s11060-009-9861-0.
- Takai K., Taniguchi M., Takahashi H., Usui M., Saito N. Comparative analysis of spinal hemangioblastomas in sporadic disease and von Hippel–Lindau syndrome. Neurol Med Chir (Tokyo) 2010; 50(7): 560–567, https://doi.org/10.2176/nmc.50.560.
- Park C.H., Lee C.H., Hyun S.J., Jahng T.A., Kim H.J., Kim K.J. Surgical outcome of spinal cord hemangioblastomas. J Korean Neurosurg Soc 2012; 52(3): 221–227, https://doi.org/10.3340/jkns.2012.52.3.221.
- Sadashivam S., Abraham M., Kesavapisharady K., Nair S.N. Long-term outcome and prognostic factors of intramedullary spinal hemangioblastomas. Neurosurg Rev 2020; 43(1): 169–175, https://doi.org/10.1007/s10143-018-1025-2.
- Cristante L., Herrmann H.D. Surgical management of intramedullary hemangioblastoma of the spinal cord. Acta Neurochir (Wien) 1999; 141(4): 333–340, https://doi.org/10.1007/s007010050308.
- Lonser R.R., Weil R.J., Wanebo J.E., DeVroom H.L., Oldfield E.H. Surgical management of spinal cord hemangioblastomas in patients with von Hippel–Lindau disease. J Neurosurg 2003; 98(1): 106–116, https://doi.org/10.3171/jns.2003.98.1.0106.
- Lee D.K., Choe W.J., Chung C.K., Kim H.J. Spinal cord hemangioblastoma: surgical strategy and clinical outcome. J Neurooncol 2003; 61(1): 27–34, https://doi.org/10.1023/a:1021297622944.
- Bostrom A., Hans F.J., Reinacher P.C., Krings T., Burgel U., Gilsbach J.M., Reinges M.H.T. Intramedullary hemangioblastomas: timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J 2008; 17(6): 882–886, https://doi.org/10.1007/s00586-008-0658-1.
- Shin D.A., Kim S.H., Kim K.N., Shin H.C., Yoon D.H. Surgical management of spinal cord haemangioblastoma. Acta Neurochir (Wien) 2008; 150(3): 215–220, https://doi.org/10.1007/s00701-008-1396-6.
- Mandigo C.E., Ogden A.T., Angevine P.D., McCormick P.C. Operative management of spinal hemangioblastoma. Neurosurgery 2009; 65(6): 1166–1177, https://doi.org/10.1227/01.neu.0000359306.74674.c4.
- Clark A.J., Lu D.C., Richardson R.M., Tihan T., Parsa A.T., Chou D., Barbaro N.M., Kunwar S., Weinstein P.R., Lawton M.T., Berger M.S., McDermott M.W. Surgical technique of temporary arterial occlusion in the operative management of spinal hemangioblastomas. World Neurosurg 2010; 74(1): 200–205, https://doi.org/10.1016/j.wneu.2010.03.016. Ghobrial G.M., Liounakos J., Starke R.M., Levi A.D. Surgical treatment of vascular intramedullary spinal cord lesions. Cureus 2018; 10(8): e3154, https://doi.org/10.7759/cureus.3154.
- Kruger M.T., Steiert C., Glasker S., Klingler J.H. Minimally invasive resection of spinal hemangioblastoma: feasibility and clinical results in a series of 18 patients. J Neurosurg Spine 2019; 31(6): 880–889, https://doi.org/10.3171/2019.5.spine1975.
- Ozkan E., Gupta S. Embolization of spinal tumors: vascular anatomy, indications, and technique. Tech Vasc Interv Radiol 2011; 14(3): 129–140, https://doi.org/10.1053/j.tvir.2011.02.005.
- Berenstein A., Lasjaunias P., Brugge K.G. Tumors of the spinal column and spinal cord. In: Surgical neuroangiography: clinical and endovascular treatment aspects in adults. vol. 2. Springer, Berlin, Heidelberg; 2004; p. 874–877.
- Griessenauer C.J., Salem M., Hendrix P., Foreman P.M., Ogilvy C.S., Thomas A.J. Preoperative embolization of spinal tumors: a systematic review and meta-analysis. World Neurosurg 2016; 87: 362–371, https://doi.org/10.1016/j.wneu.2015.11.064.
- Derdeyn C.P., Moran C.J., Cross D.T., Dietrich H.H., Dacey R.G. Jr. Polyvinyl alcohol particle size and suspension characteristics. AJNR Am J Neuroradiol 1995; 16(6): 1335–1343.
- Bhatia K.D., Wang L., Parkinson R.J., Wenderoth J.D. Successful treatment of six cases of indirect carotid-cavernous fistula with ethylene vinyl alcohol copolymer (Onyx) transvenous embolization. J Neuroophthalmol 2009; 29(1): 3–8, https://doi.org/10.1097/wno.0b013e318199c85c.
- Mindea S.A., Eddleman C.S., Hage Z.A., Batjer H.H., Ondra S.L., Bendok B.R. Endovascular embolization of a recurrent cervical giant cell neoplasm using N-butyl 2-cyanoacrylate. J Clin Neurosci 2009; 16(3): 452–454, https://doi.org/10.1016/j.jocn.2008.03.017.
- Hu Y.C., Newman C.B., Dashti S.R., Albuquerque F.C., McDougall C.G. Cranial dural arteriovenous fistula: transarterial Onyx embolization experience and technical nuances. J Neurointerv Surg 2011; 3(1): 5–13, https://doi.org/10.1136/jnis.2010.003707.
- Ampie L., Choy W., Khanna R., Smith Z.A., Dahdaleh N.S., Parsa A.T., Bloch O. Role of preoperative embolization for intradural spinal hemangioblastomas. J Clin Neurosci 2016; 24: 83–87, https://doi.org/10.1016/j.jocn.2015.09.006.
- Wilson M.A., Cooke D.L., Ghodke B., Mirza S.K. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol 2010; 31(4): 656–660, https://doi.org/10.3174/ajnr.a1899.
- Saliou G., Giammattei L., Ozanne A., Messerer M. Role of preoperative embolization of intramedullary hemangioblastoma. Neurochirurgie 2017; 63(5): 372–375, https://doi.org/10.1016/j.neuchi.2016.01.004.
- Yang Y.M., Wang D.M., Jiang H.Z., Sha C., Yuan Q.G., Liu J.C. Treatment of spinal cord hemangioblastoma by microoperations combined with embolization. Zhonghua Yi Xue Za Zhi 2008; 88(19): 1309–1312.
- Biondi A., Ricciardi G.K., Faillot T., Capelle L., Van Effenterre R., Chiras J. Hemangioblastomas of the lower spinal region: report of four cases with preoperative embolization and review of the literature. AJNR Am J Neuroradiol 2005; 26(4): 936–945.
- Cornelius J.F., Saint-Maurice J.P., Bresson D., George B., Houdart E. Hemorrhage after particle embolization of hemangioblastomas: comparison of outcomes in spinal and cerebellar lesions. J Neurosurg 2007; 106(6): 994–998, https://doi.org/10.3171/jns.2007.106.6.994.
- Vazquez-Anon V., Botella C., Beltran A., Solera M., Piquer J. Preoperative embolization of solid cervicomedullary junction hemangioblastomas: report of two cases. Neuroradiology 1997; 39(2): 86–89, https://doi.org/10.1007/s002340050372.
- Standard S.C., Ahuja A., Livingston K., Guterman L.R., Hopkins L.N. Endovascular embolization and surgical excision for the treatment of cerebellar and brain stem hemangioblastomas. Surg Neurol 1994; 41(5): 405–410, https://doi.org/10.1016/0090-3019(94)90035-3.
- Awad A.W., Almefty K.K., Ducruet A.F., Turner J.D., Theodore N., McDougall C.G., Albuquerque F.C. The efficacy and risks of preoperative embolization of spinal tumors. J Neurointerv Surg 2016; 8(8): 859–864, https://doi.org/10.1136/neurintsurg-2015-011833.
- Hong C.G., Cho J.H., Suh D.C., Hwang C.J., Lee D.H., Lee C.S. Preoperative embolization in patients with metastatic spinal cord compression: mandatory or optional? World J Surg Oncol 2017; 15(1): 45, https://doi.org/10.1186/s12957-017-1118-3.
- Chen L., Li D.H., Lu Y.H., Hao B., Cao Y.Q. Preoperative embolization versus direct surgery of meningiomas: a meta-analysis. World Neurosurg 2019; 128: 62–68, https://doi.org/10.1016/j.wneu.2019.02.223.
- Tang B., Ji T., Tang X., Jin L., Dong S., Guo W. Risk factors for major complications in surgery for hypervascular spinal tumors: an analysis of 120 cases with adjuvant preoperative embolization. Eur Spine J 2015; 24(10): 2201–2218, https://doi.org/10.1007/s00586-015-4122-8.
- Tobin M.K., Geraghty J.R., Engelhard H.H., Linninger A.A., Mehta A.I. Intramedullary spinal cord tumors: a review of current and future treatment strategies. Neurosurg Focus 2015; 39(2): E14, https://doi.org/10.3171/2015.5.focus15158.
- Molina C.A., Pennington Z., Ahmed A.K., Westbroek E., Goodwin M.L., Tamargo R., Sciubba D.M. Use of intraoperative indocyanine green angiography for feeder vessel ligation and en bloc resection of intramedullary hemangioblastoma. Oper Neurosurg (Hagerstown) 2019; 17(6): 573–579, https://doi.org/10.1093/ons/opz053.
- Ferroli P., Acerbi F., Albanese E., Tringali G., Broggi M., Franzini A., Broggi G. Application of intraoperative indocyanine green angiography for CNS tumors: results on the first 100 cases. Acta Neurochir Suppl 2011; 109: 251–217, https://doi.org/10.1007/978-3-211-99651-5_40.
- Acerbi F., Vetrano I.G., Sattin T., de Laurentis C., Bosio L., Rossini Z., Broggi M., Schiariti M., Ferroli P. The role of indocyanine green videoangiography with FLOW 800 analysis for the surgical management of central nervous system tumors: an update. Neurosurg Focus 2018; 44(6): E6, https://doi.org/10.3171/2018.3.focus1862.
- Zelken J.A., Tufaro A.P. Current trends and emerging future of indocyanine green usage in surgery and oncology: an update. Ann Surg Oncol 2015; 22 Suppl 3: S1271–S1283, https://doi.org/10.1245/s10434-015-4743-5.
- Hwang S.W., Malek A.M., Schapiro R., Wu J.K. Intraoperative use of indocyanine green fluorescence videography for resection of a spinal cord hemangioblastoma. Neurosurgery 2010; 67(3 Suppl Operative): ons300–ons303, https://doi.org/10.1227/01.neu.0000383876.72704.7b.
- Schubert G.A., Schmieder K., Seiz-Rosenhagen M., Thome C. ICG videography facilitates interpretation of vascular supply and anatomical landmarks in intramedullary spinal lesions: two case reports. Spine (Phila Pa 1976) 2011; 36(12): E811–E813, https://doi.org/10.1097/brs.0b013e3181fd6557.
- Ueba T., Abe H., Matsumoto J., Higashi T., Inoue T. Efficacy of indocyanine green videography and real-time evaluation by FLOW 800 in the resection of a spinal cord hemangioblastoma in a child: case report. J Neurosurg Pediatr 2012; 9(4): 428–431, https://doi.org/10.3171/2011.12.peds11286.
- Hao S., Li D., Ma G., Yang J., Wang G. Application of intraoperative indocyanine green videoangiography for resection of spinal cord hemangioblastoma: advantages and limitations. J Clin Neurosci 2013; 20(9): 1269–1275, https://doi.org/10.1016/j.jocn.2012.12.008.
- Takami T., Yamagata T., Naito K., Arima H., Ohata K. Intraoperative assessment of spinal vascular flow in the surgery of spinal intramedullary tumors using indocyanine green videoangiography. Surg Neurol Int 2013; 4: 135, https://doi.org/10.4103/2152-7806.119352.
- Takami T., Naito K., Yamagata T., Shimokawa N., Ohata K. Benefits and limitations of indocyanine green fluorescent image-guided surgery for spinal intramedullary tumors. Oper Neurosurg (Hagerstown) 2017; 13(6): 746–754, https://doi.org/10.1093/ons/opx057.










