Cellular and Molecular Mechanisms of Toxic Liver Fibrosis in Rats Depending on the Stages of Its Development
The aim is to study the cellular and molecular features of toxic liver fibrosis in rats and its dependence on development stages of this pathological condition.
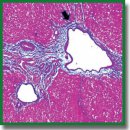
Materials and Methods. Liver fibrogenesis in male Wistar rats was induced with the thioacetamide solution by introducing into the stomach with a probe at a dose of 200 mg/kg of animal body weight 2 times per week. The process dynamics was studied at 5 time points (control, week 3, week 5, week 7, and week 9). The mRNA levels of tweak, fn14, ang, vegfa, cxcl12, and mmp-9 genes in liver were detected by real-time polymerase chain reaction. Immunohistochemical study was performed on paraffin sections. The CD31, CD34, CK19, α-SMA, FAP, CD68, CD206, CX3CR1, and CD45 cells were used as markers. Fibrosis degree was determined in histological sections, stained in line with the Mallory technique, according to the Ishak’s semi-quantitative scale.
Results. Two simultaneously existing morphologically heterogeneous populations of myofibroblasts expressing different types of markers (FAP, α-SMA) were identified in rat liver. Prior to the onset of transformation of fibrosis into cirrhosis (F1–F4, weeks 3–7), FAP+ and SMA+ cells were localized in different places on histological specimens. All stages of liver fibrosis development were accompanied by an increase in the number (p=0.0000), a change in the phenotypic structure and functional properties of macrophages. The CK19+ cells of the portal areas differentiated into cholangiocytes that formed interlobular bile ducts and ductules, as well as hepatocytes that formed rudiments of new hepatic microlobules. Pathological venous angiogenesis and heterogeneity of endotheliocytes of the intrahepatic vascular bed were detected. Two options for changes in mRNA expression of the selected genes were identified. The level of the fn14 and mmp-9 mRNAs at all stages of fibrosis was higher (p=0.0000) than in control rats. For tweak, ang, vegfa, and cxcl12 mRNAs, the situation was the opposite — the level of genes decreased (p=0.0000). There were strong and moderate correlations between the studied target genes (p<0.05).
Conclusion. It was established that the stages of toxic fibrosis had morphological and molecular genetic features. The FAP+ cells make the main contribution to development of portal and initial stage of bridging fibrosis. The stellate macrophages and infiltrating monocytes/macrophages can potentially be used for development of new therapeutic strategies for liver pathology treatment. One should take into account the features of the markers’ expression by endothelial cells during the study of the intrahepatic vascular bed. Joint study of genes is a necessary ad-hoc parameter in fundamental and preclinical research.
- Asrani S.K., Devarbhavi H., Eaton J., Kamath P.S. Burden of liver diseases in the world. J Hepatol 2019; 70(1): 151–171, https://doi.org/10.1016/j.jhep.2018.09.014.
- Roehlen N., Crouchet E., Baumert T.F. Liver fibrosis: mechanistic concepts and therapeutic perspectives. Cells 2020; 9(4): 875, https://doi.org/10.3390/cells9040875.
- Xu M., Xu H.H., Lin Y., Sun X., Wang L.J., Fang Z.P., Su X.H., Liang X.J., Hu Y., Liu Z.M., Cheng Y., Wei Y., Li J., Li L., Liu H.J., Cheng Z., Tang N., Peng C., Li T., Liu T., Qiao L., Wu D., Ding Y.Q., Zhou W.J. LECT2, a ligand for Tie1, plays a crucial role in liver fibrogenesis. Cell 2019; 178(6): 1478–1492.e20, https://doi.org/10.1016/j.cell.2019.07.021.
- Friedman S.L., Pinzani M. Hepatic fibrosis 2022: unmet needs and a blueprint for the future. Hepatology 2022; 75(2): 473–488, https://doi.org/10.1002/hep.32285.
- Lin Y., Dong M.Q., Liu Z.M., Xu M., Huang Z.H., Liu H.J., Gao Y., Zhou W.J. A strategy of vascular-targeted therapy for liver fibrosis. J Hepatology 2022; 76(3): 660–675, https://doi.org/10.1002/hep.32299.
- Zhang D., Zhang Y., Sun B. The molecular mechanisms of liver fibrosis and its potential therapy in application. Int J Mol Sci 2022; 23(20): 12572, https://doi.org/10.3390/ijms232012572.
- Borrello M.T., Mann D. Chronic liver diseases: from development to novel pharmacological therapies: IUPHAR review 37. Br J Pharmacol 2022, https://doi.org/10.1111/bph.15853.
- Jangra A., Kothari A., Sarma P., Medhi B., Omar B.J., Kaushal K. Recent advancements in antifibrotic therapies for regression of liver fibrosis. Cells 2022; 11(9): 1500, https://doi.org/10.3390/cells11091500.
- Li Y., Yuan S.L., Yin J.Y., Yang K., Zhou X.G., Xie W., Wang Q. Differences of core genes in liver fibrosis and hepatocellular carcinoma: evidence from integrated bioinformatics and immunohistochemical analysis. World J Gastrointest Oncol 2022; 14(7): 1265–1280, https://doi.org/10.4251/wjgo.v14.i7.1265.
- Antar S.A., Ashour N.A., Marawan M.E., Al-Karmalawy A.A. Fibrosis: types, effects, markers, mechanisms for disease progression, and its relation with oxidative stress, immunity, and inflammation. Int J Mol Sci 2023; 24(4): 4004, https://doi.org/10.3390/ijms24044004.
- Parola M., Pinzani M. Liver fibrosis: pathophysiology, pathogenetic targets and clinical issues. Mol Aspects Med 2019; 65: 37–55, https://doi.org/10.1016/j.mam.2018.09.002.
- Li H. Angiogenesis in the progression from liver fibrosis to cirrhosis and hepatocelluar carcinoma. Expert Rev Gastroenterol Hepatol 2021; 15(3): 217–233, https://doi.org/10.1080/17474124.2021.1842732.
- Yang L., Yue W., Zhang H., Zhang Z., Xue R., Dong C., Liu F., Chang N., Yang L., Li L. Dual targeting of Angipoietin-1 and von Willebrand factor by microRNA-671-5p attenuates liver angiogenesis and fibrosis. Hepatol Commun 2022; 6(6): 1425–1442, https://doi.org/10.1002/hep4.1888.
- Wallace S.J., Tacke F., Schwabe R.F., Henderson N.C. Understanding the cellular interactome of non-alcoholic fatty liver disease. JHEP Rep 2022; 4(8): 100524, https://doi.org/10.1016/j.jhepr.2022.100524.
- Quintero-Fabián S., Arreola R., Becerril-Villanueva E., Torres-Romero J.C., Arana-Argáez V., Lara-Riegos J., Ramírez-Camacho M.A., Alvarez-Sánchez M.E. Role of matrix metalloproteinases in angiogenesis and cancer. Front Oncol 2019; 9: 1370, https://doi.org/10.3389/fonc.2019.01370.
- Hoeben A., Landuyt B., Highley M.S., Wildiers H., Van Oosterom A.T., De Bruijn E.A. Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 2004; 56(4): 549–580, https://doi.org/10.1124/pr.56.4.3.
- Jones M.L., Ewing C.M., Isaacsa W.B., Getzenberg R.H. Prostate cancer-derived angiogenin stimulates the invasion of prostate fibroblasts. J Cell Mol Med 2012; 16(1): 193–201, https://doi.org/10.1111/j.1582-4934.2011.01283.x.
- Wang M., Xie Z., Xu J., Feng Z. TWEAK/Fn14 axis in respiratory diseases. Clin Chim Acta 2020; 509: 139–148, https://doi.org/10.1016/j.cca.2020.06.007.
- Dwyer B.J., Jarman E.J., Gogoi-Tiwari J., Ferreira-Gonzalez S., Boulter L., Guest R.V., Kendall T.J., Kurian D., Kilpatrick A.M., Robson A.J., O’Duibhir E., Man T.Y., Campana L., Starkey Lewis P.J., Wigmore S.J., Olynyk J.K., Ramm G.A., Tirnitz-Parker J.E.E., Forbes S.J. TWEAK/Fn14 signalling promotes cholangiocarcinoma niche formation and progression. J Hepatol 2021; 74(4): 860–872, https://doi.org/10.1016/j.jhep.2020.11.018.
- Short C., Zhong A., Xu J., Mahdi E., Glazier A., Malkoff N., Noriega N., Yeo T., Asahina K., Wang K.S. TWEAK/FN14 promotes profibrogenic pathway activation in Prominin-1-expressing hepatic progenitor cells in biliary atresia. Hepatology 2023; 77(5): 1639–1653, https://doi.org/10.1097/hep.0000000000000026.
- Dhar D., Baglieri J., Kisseleva T., Brenner D.A. Mechanisms of liver fibrosis and its role in liver cancer. Exp Biol Med (Maywood) 2020; 245(2): 96–108, https://doi.org/10.1177/1535370219898141.
- Luo N., Li J., Wei Y., Lu J., Dong R. Hepatic stellate cell: a double-edged sword in the liver. Physiol Res 2021; 70(6): 821–829, https://doi.org/10.33549/physiolres.934755.
- Cheng D., Chai J., Wang H., Fu L., Peng S., Ni X. Hepatic macrophages: key players in the development and progression of liver fibrosis. Liver Int 2021; 41(10): 2279–2294, https://doi.org/10.1111/liv.14940.
- Wang C., Ma C., Gong L., Guo Y., Fu K., Zhang Y., Zhou H., Li Y. Macrophage polarization and its role in liver disease. Front Immunol 2021; 12: 803037, https://doi.org/10.3389/fimmu.2021.803037.
- Lafoz E., Ruart M., Anton A., Oncins A., Hernández-Gea V. The endothelium as a driver of liver fibrosis and regeneration. Cells 2020; 9(4): 929, https://doi.org/10.3390/cells9040929.
- Zadorozhna M., Di Gioia S., Conese M., Mangieri D. Neovascularization is a key feature of liver fibrosis progression: anti-angiogenesis as an innovative way of liver fibrosis treatment. Mol Biol Rep 2020; 47(3): 2279–2288, https://doi.org/10.1007/s11033-020-05290-0.
- Kumar S., Duan Q., Wu R., Harris E.N., Su Q. Pathophysiological communication between hepatocytes and non-parenchymal cells in liver injury from NAFLD to liver fibrosis. Adv Drug Deliv Rev 2021; 176: 113869, https://doi.org/10.1016/j.addr.2021.113869.
- Banin V.V., Belousova T.A., Bykov V.L. Terminologia Histologica. Mezhdunarodnye terminy po tsitologii i gistologii cheloveka s ofitsial’nym spiskom russkikh ekvivalentov: spravochnoe posobie [Terminologia Histologica. International terms in human cytology and histology with the official list of Russian equivalents: a reference guide]. Banin V.V., Bykov V.L. (editors). Moscow: GEOTAR-Media; 2009; 272 p.
- Muthiah M.D., Huang D.Q., Zhou L., Jumat N.H., Choolani M., Chan J.K.Y., Wee A., Lim S.G., Dan Y.Y. A murine model demonstrating reversal of structural and functional correlates of cirrhosis with progenitor cell transplantation. Sci Rep 2019; 9(1): 15446, https://doi.org/10.1038/s41598-019-51189-7.
- Teoreticheskie osnovy i prakticheskoe primenenie metodov immunogistokhimii [Theoretical bases and practical application of immunohistochemistry methods]. Korzhevskii D.E. (editor). Saint Petersburg: SpetsLit; 2014; 119 p.
- Zheng C., Luo J., Yang Y., Dong R., Yu F.X., Zheng S. YAP activation and implications in patients and a mouse model of biliary atresia. Front Pediatr 2021; 8: 618226, https://doi.org/10.3389/fped.2020.618226.
- Everhart J.E., Wright E.C., Goodman Z.D., Dienstag J.L., Hoefs J.C., Kleiner D.E., Ghany M.G., Mills A.S., Nash S.R., Govindarajan S., Rogers T.E., Greenson J.K., Brunt E.M., Bonkovsky H.L., Morishima C., Litman H.J.; HALT-C Trial Group. Prognostic value of Ishak fibrosis stage: findings from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology 2010; 51(2): 585–594, https://doi.org/10.1002/hep.23315.
- Lebedeva E.I., Babenko A.S., Shchastniy A.T. Stability of the sdha, hprt, prl3d1 and hes1 gene expression in a rat liver fibrosis model. Biomedicine 2022; 18(2): 17–30, https://doi.org/10.33647/2074-5982-18-2-17-30.
- Younis N.S., Ghanim A.M.H., Elmorsy M.A., Metwaly H. Taurine ameliorates thioacetamide induced liver fibrosis in rats via modulation of toll like receptor 4/nuclear factor kappa B signaling pathway. Sci Rep 2021; 11(1): 12296, https://doi.org/10.1038/s41598-021-91666-6.
- Wu Y., Li Z., Xiu A.Y. Meng D.X., Wang S.N., Zhang C.Q. Carvedilol attenuates carbon tetrachloride-induced liver fibrosis and hepatic sinusoidal capillarization in mice. Drug Des Devel Ther 2019; 13: 2667–2676, https://doi.org/10.2147/dddt.s210797.
- Yang A.T., Kim Y.O., Yan X.Z., Abe H., Aslam M., Park K.S., Zhao X.Y., Jia J.D., Klein T., You H., Schuppan D. Fibroblast activation protein activates macrophages and promotes parenchymal liver inflammation and fibrosis. Cell Mol Gastroenterol Hepatol 2023; 15(4): 841–867, https://doi.org/10.1016/j.jcmgh.2022.12.005.
- Fuji H., Miller G., Nishio T., Koyama Y., Lam K., Zhang V., Loomba R., Brenner D., Kisseleva T. The role of mesothelin signaling in portal fibroblasts in the pathogenesis of cholestatic liver fibrosis. Front Mol Biosci 2021; 8: 790032, https://doi.org/10.3389/fmolb.2021.790032.
- Dong X., Liu J., Xu Y., Cao H. Role of macrophages in experimental liver injury and repair in mice. Exp Ther Med 2019; 17(5): 3835–3847, https://doi.org/10.3892/etm.2019.7450.
- Kamimoto K., Nakano Y., Kaneko K., Miyajima A., Itoh T. Multidimensional imaging of liver injury repair in mice reveals fundamental role of the ductular reaction. Commun Biol 2020; 3(1): 289, https://doi.org/10.1038/s42003-020-1006-1.
- Sato K., Marzioni M., Meng F., Francis H., Glaser S., Alpini G. Ductular reaction in liver diseases: pathological mechanisms and translational significances. Hepatology 2019; 69(1): 420–430, https://doi.org/10.1002/hep.30150.
- Augustin H.G., Koh G.Y. Organotypic vasculature: from descriptive heterogeneity to functional pathophysiology. Science 2017; 357(6353): eaal2379, https://doi.org/10.1126/science.aal2379.
- Zhou W., Guo S., Liu M., Burow M.E., Wang G. Targeting CXCL12/CXCR4 axis in tumor immunotherapy. Curr Med Chem 2019; 26(17): 3026–3041, https://doi.org/10.2174/0929867324666170830111531.
- Zhang Y., Zeng W., Xia Y. TWEAK/Fn14 axis is an important player in fibrosis. J Cell Physiol 2021; 236(5): 3304–3316, https://doi.org/10.1002/jcp.30089.










