Prediction of Hospital Mortality in Patients with ST Segment Elevation Myocardial Infarction: Evolution of Risk Measurement Techniques and Assessment of Their Effectiveness (Review)
Risk stratification of hospital mortality in patients with ST segment elevation myocardial infarction on the electrocardiogram is an important part of the specialized medical care provision. The systematic review presents scientific literature data characterizing the predictive value of both classical prognostic scales (GRACE, CADDILLAC, TIMI risk score for STEMI, RECORD, etc.) and new risk measurement tools developed on the basis of modern machine learning techniques. Most studies on this issue are often focused on the search for new predictors of adverse events, which allow to detail the relations between indicators of the clinical and functional status of patients and the end point of the study. Here, an important task is to develop hospital mortality prognostic algorithms characterized by explainable artificial intelligence and trusted by doctors.
Introduction
Coronary heart disease (CHD) is the most spread cause of disability and mortality in most countries worldwide. ST segment elevation myocardial infarction on the electrocardiogram (STEMI) is the most severe clinical form of CHD and is associated with a high risk of adverse outcomes, including hospital mortality (HM). In the Russian Federation, the HM rate for STEMI varies within 13–14%, which is comparable to European countries and indicates the need to improve risk measurement tools that allow timely assess the likelihood of adverse events [1]. To assess the risk of HM in patients with STEMI, there were over 50 scales and prognostic algorithms developed in different countries, some of which are recommended by professional communities for common use and proved their effectiveness in real clinical practice [2–61]. Such scales include GRACE (Global Registry of Acute Coronary Events), CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications), TIMI risk score for STEMI (Thrombolysis in Myocardial Infarction risk score for ST segment elevation myocardial infarction), RECORD, and etc. [3–6]. Currently, the research is ongoing with the aim to find new HM predictors, which add-up to the structure of earlier developed “classical” scales to increase the prediction accuracy. Also, constant expansion of STEMI patient registries requires modern machine learning (ML) techniques to process and analyze big data. This brings up new knowledge that provides details on the relations of potential predictors to the study end point. Predictive algorithms based on ML techniques are increasingly used to assess the risk of adverse events in various areas of clinical medicine, thus their quality improvement is the subject of multiple studies.
The aim of this review is to analyze scientific publications on prediction of hospital mortality in patients with STEMI and to assess the possibility to improve risk measurement tools based on modern machine learning techniques.
Literature sources
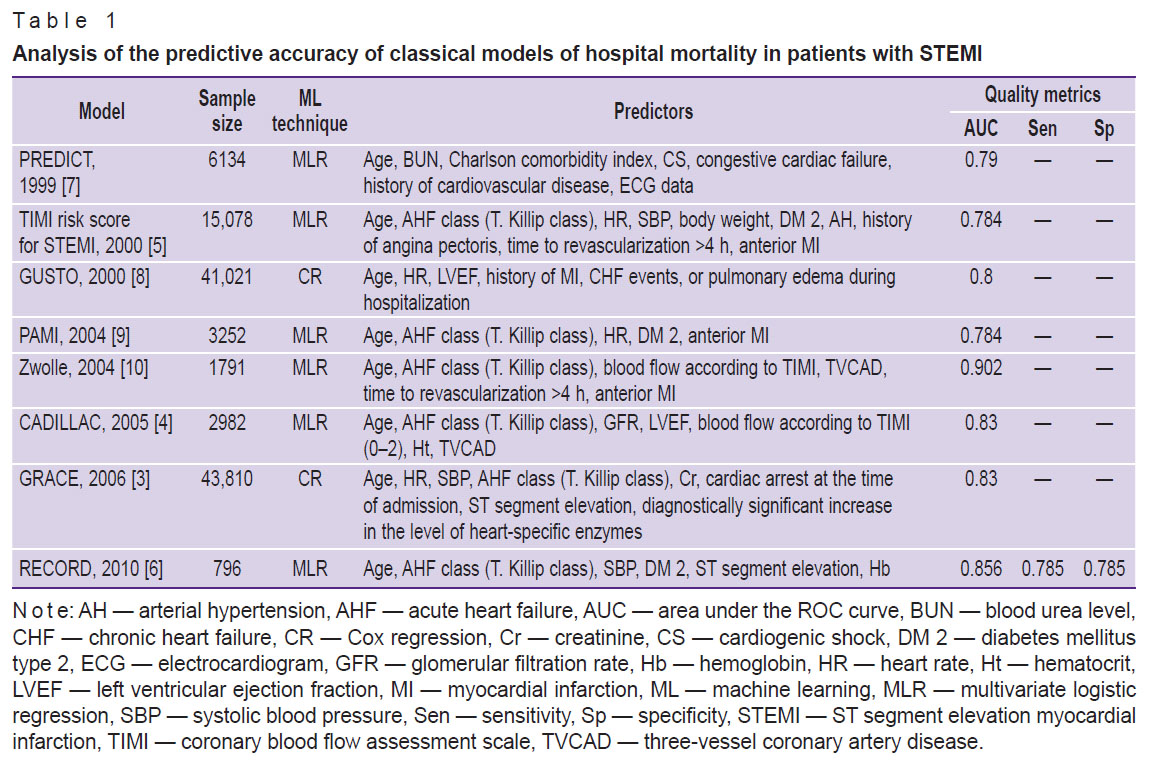
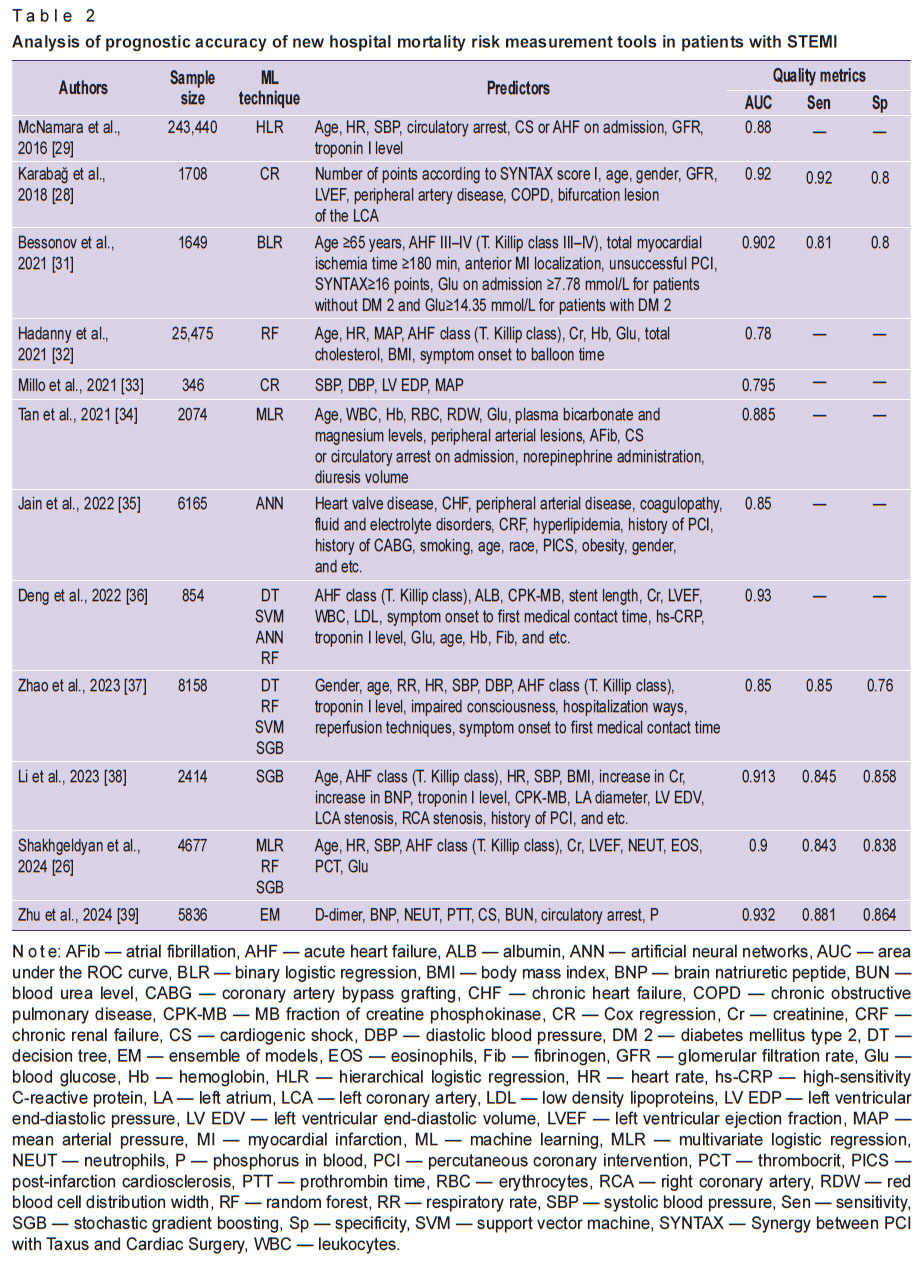
Literature sources were searched in the PubMed (MEDLINE), Web of Science, Scopus, eLIBRARY.RU and Cochrane Database of Systematic Reviews databases using the following key words: “ST segment elevation myocardial infarction and mortality”, “ST segment elevation myocardial infarction and prognostic scales”, “ST segment elevation myocardial infarction and prognosis”, “scale prognosis of in-hospital mortality and TEMI”, “ST segment elevation myocardial infarction and prognosis scale in hospital mortality”. Based on the query results, 46,134 documents were selected. Duplicates were removed and the following documents were excluded: the documents that did not contain the data required for analysis (techniques to develop predictive models, indicators of their accuracy, information about predictors); the freely available documents with full-text materials; and studies with insufficient sample size (<200). The final version of the systematic review included 102 documents published during the period from 1999 to 2024. The most cited documents are provided in Tables 1 and 2.
“Classical” scales to predict the risk of hospital mortality in patients with STEMI
Active scientific work associated with the development of prognostic scales to stratify the risk of HM in patients with acute forms of CHD has been ongoing since the end of the last century and is caused by two main reasons: the increasing morbidity and mortality of the population from cardiovascular diseases in most countries worldwide and the intensive development of ML techniques. To develop prognostic ML models in clinical medicine, multivariate logistic regression (MLR), Cox regression (CR), random forest (RF), decision tree (DT), artificial neural networks (ANN), stochastic gradient boosting (SGB), support vector machines (SVM) and ensembles of models are most often used [62–66].
The PREDICT scale, which was one of the first scales introduced to the professional community, was developed in 1999 based on the results of the Minnesota Heart Study (MHS), which included data from 6134 patients from the acute coronary syndrome (ACS) registry, and was validated on a sample of 3570 patients with STEMI [7]. The MLR-based prognostic algorithm demonstrated acceptable accuracy in predicting HM (AUC — 0.79).
In 2000, the TIMI risk score for STEMI was developed based on the data from the InTIME II registry, which contained the results of examination and treatment of 15,078 patients with STEMI [5]. The scale included HM predictors, which were further used in other risk measurement tools and are still relevant. These predictors include the age of the patients, the T. Killip class of acute heart failure (AHF), heart rate (HR), and systolic blood pressure (SBP). The combination of these indicators with such factors as diabetes mellitus type 2 (DM 2), arterial hypertension (AH), body weight, history of angina pectoris, time to revascularization >4 h, and myocardial infarction (MI) localization allowed to prepare acceptable prognosis accuracy (AUC — 0.784); this became the basis for future research. The scale was validated with data of 3687 patients with STEMI in the TIMI-9 study, whereas the HM probability was stratified into low, intermediate, and high risk groups.
The GUSTO scale was developed in 2000 based on the results of a similarly named multicenter study that contained data of 41,021 patients with STEMI [8]. A prognostic algorithm based on CR, in addition to the age of patients, HR, MI localization, and indicators of chronic heart failure (CHF), first included an indicator of left ventricular ejection fraction (LVEF). At that, this factor in the model structure did not ensure the expected increase in the model accuracy (AUC — 0.8), which was comparable to algorithms without this predictor. The prognostic “neutrality” of the LVEF factor in this model can be explained by the fact that it lacks categorization that specifies threshold values enhancing the predictive potential [67].
The PAMI scale, introduced in 2004 and based on 4 registries of patients with STEMI, was not more accurate than the previously developed prognostic tools [9]. Predictors of the MLR prognostic model included the age of patients, AHF class (T. Killip class), heart rate, DM 2, and MI location. Indicators with a previously proven link to HM in the algorithm structure ensured its acceptable predictive accuracy, comparable to the TIMI risk score for STEMI (AUC — 0.784).
The authors of the Zwolle scale (2004) [10] were the first to draw attention to the prognostic value of such potential HM predictors as triple vessel coronary artery disease (TVCAD) and the degree of restoration of coronary blood flow according to TIMI. The combination of these factors with the indicators of age, AHF class (T. Killip class), time to myocardial revascularization >4 h, and anterior MI demonstrated excellent predictive accuracy (AUC — 0.902).
The CADILLAC scale, developed in 2005 based on analysis of data from the registry with the same name and validated on a cohort of patients from the Stent-PAMI study, combined predictors of HM and annual mortality in patients with STEMI in its structure [4]. The prognostic algorithm based on MLR included indicators of patients’ age, AHF class (T. Killip class), glomerular filtration rate (GFR), LVEF, indicators of coronary blood flow restoration according to TIMI, hematocrit (Ht), and TVCAD. GFR and Ht indicators were first applied as HM predictors and were subsequently used in other prognostic algorithms. The CADILLAC score demonstrated appropriate predictive accuracy for HM, including in patients with STEMI after percutaneous coronary intervention (PCI) (AUC — 0.83) [4].
The GRACE scale was developed in 2006 using CR and was based on the data from the similarly named international registry of patients with ACS that contains information about 43,810 patients (21,688 — a sample for training the model, 22,122 — a sample for the model validation), and was subsequently recommended for clinical use in most countries worldwide [3]. The structure of the scale included previously known HM predictors: patients’ age, HR, SBP, AHF class (T. Killip class), as well as indicators of creatinine (Cr) concentration in the blood serum, ST segment elevation, diagnostically significant increase in the level of heart-specific enzymes, and cardiac arrest at the patient’s admission to hospital.
The advantage of the GRACE scale is the combination of appropriate predictive accuracy (AUC — 0.83) and availability of predictors for HM risk stratification (low, medium, and high). The version of the scale updated in 2014 (GRACE 2.0) allows to assess the risk of mortality 1 and 3 years after ACS [11]. In a number of studies, modification of the GRACE scale was made by adding new HM risk factors to its structure [12–23]. The most accurate prognosis (AUC — 0.927) was made by a model the predictors of which included LVEF and blood leukocyte content [24].
The first Russian risk measurement tool to assess HM probability in patients with STEMI was the RECORD scale, developed in 2010 on the basis of univariate logistic regression and MLR on data from 796 ACS patients from regional medical institutions included in the similarly named register [6]. The scale structure included six predictors: patients’ age, AHF class (T. Killip class), SBP, DM 2, ST segment elevation, and hemoglobin (Hb) content in blood. HM likelihood was stratified into low-risk and high-risk groups. Available predictors and the appropriate level of predictive accuracy (AUC — 0.856) are the main advantages of the scale. Its disadvantages include the lack of validation on large independent samples. Evaluation of HM risk in patients with STEMI, which was made at the prehospital stage, was conducted using a modified RECORD algorithm with no Hb indicator in the structure, which did not reduce the predictive accuracy [25].
New hospital mortality risk measurement tools for patients with STEMI
Improved quality of prognostic algorithms is related to the use of explainable artificial intelligence techniques, which allow to develop interpretable ML models that provide for clinical justification for the generated conclusion [26]. Their importance increases when predicting HM after emergency myocardial revascularization. This is due to the need to assess the degree of coronary damage, which is made according to SYNTAX score I (SS I), developed in 2006, and SYNTAX score II (SS II), presented in 2013 [27, 68]. The complex of SS II predictors, in addition to anatomical indicators of coronary blood flow violations, contains clinical and anamnestic data of patients: age, gender, GFR, LVEF, damage to peripheral arteries, history of chronic obstructive pulmonary disease. Recently, the number of publications in which the SS II scale is used to predict HM in patients with STEMI has increased. These include Karabağ et al. [28], where excellent predictive accuracy of HM after PCI was demonstrated (AUC — 0.92). Prognostic algorithms for HM prior to PCI were shown by McNamara et al. [29]. These algorithms, which were developed on data from the ACTION registry (243,440 patients with ACS) using hierarchical logistic regression, had equivalent accuracy in groups of patients with STEMI and NSTEMI (AUC — 0.88). Based on the prediction results, HM probability was stratified into 5 risk degrees, the lowest corresponding to 0.4%, and the highest — to 49.5%.
The interlink between HM and the effectiveness of thrombolytic therapy (TLT) was assessed using the EERIAM-HCC scale in [30]. The model was developed using an ensemble of ML techniques and demonstrated excellent predictive accuracy (AUC — 0.92). The greatest influence on HM was made by the indicator of continuous blood glucose concentration (Glu) and the categorical indicator of the QT interval >60 ms.
In [31], the authors presented a prognostic model of HM after PCI based on binary logistic regression, which was based on 7 predictors, including the duration of general myocardial ischemia and signs of PCI failure. The predictive algorithm had excellent accuracy (AUC — 0.902).
Based on analysis of data from 2782 patients with STEMI from the ACS registry (ACSIS), using the RF technique, Hadanny et al. [32] developed a prognostic model of HM after PCI, which was validated on 22,693 patients with STEMI (MINAP ACS registry). The model was based on 10 predictors, including the symptom onset to balloon time. Despite the scale structure having known factors of unfavorable outcome, it corresponded to only acceptable predictive accuracy (AUC — 0.78).
Millo et al. [33] used a cohort of 346 patients with STEMI aged over 60 years and developed the LASH score to assess the risk of HM after PCI. In this study, the authors used central hemodynamic monitoring data, including mean arterial pressure and left ventricular end-diastolic pressure after PCI in combination with SBP and DBP parameters, to model HM prognosis. When compared with the TIMI risk score for STEMI and GRACE algorithms, this scale demonstrated lower predictive accuracy (AUC — 0.881 for TIMI risk score for STEMI and 0.847 for GRACE vs 0.795 for LASH). Despite lower values of the quality metrics, this scale may be useful to assess the HM risk in patients with STEMI and cardiogenic shock, when indicators of the current hemodynamic status are of key importance for the prognosis. This approach was further supported by Tan et al. [34] based on data from 2074 patients with STEMI and NSTEMI from the eICU-CRD registry. Based on MLR, the HM prognostic model was developed for intensive care units (ICU) and validated on 1026 patients from the MIMIC-III database. The model included 14 HM predictors, 2 factors of which had the greatest impact on the end point: circulatory arrest (CA — 3.87) and the use of norepinephrine to stabilize hemodynamics (CA — 2). This model was superior in predictive accuracy to classical risk measurement scales used in ICUs (AUC — 0.885 vs 0.86 for SAPS II, 0.84 for OASIS, and 0.81 for SOFA).
Special attention should be paid to Jain et al. [35], who studied data from 6165 patients with STEMI aged 18 to 44 years. The ANN-based HM prediction model developed in this study had appropriate accuracy (AUC — 0.85) and was based on 22 predictors, first including tobacco smoking, alcohol abuse, drug addiction, and depression. Here, 2 factors were of utmost importance for the fatal event: damage to heart valves and fluid and electrolyte disorders.
Deng et al. [36] used DT, RF, SVM, and ANN techniques to build HM models on data from 854 patients with STEMI after PCI. In this study, an additional end point was the incidence of unrestored coronary blood flow after PCI. RF-based models had excellent predictive accuracy for HM (AUC — 0.93) and acceptable predictive accuracy for no-reflow (AUC — 0.78). Zhao et al. [37] used data of 8158 patients with STEMI to develop HM prognostic models based on 4 ML techniques (DT, RF, SVM, SGB). In addition to HM classical factors, hospitalization routes, reperfusion therapy techniques (primary PCI, TLT, TLT + PCI, no therapy), and symptom to first medical contact time were considered as predictors. Models based on SVM had the best accuracy for HM prediction (AUC — 0.85).
The greatest influence on the end point was made by reperfusion therapy techniques, patients’ age and SBP, and the least — by the symptom to first medical contact time and impaired consciousness signs. Reverse results were seen in [38], where the authors, based on SGB model, demonstrated that the impact of age, AHF class (T. Killip class), and SBP on HM is less significant than BMI, concentration of brain natriuretic peptide (BNP), and left atrial diameter. In this study, the predictive value of HR and Cr factors was predominant.
In [26], based on MLR, RF, and SGB, HM prognostic models were developed for various stages of medical care (before and after emergency PCI) with appropriate (AUC — 0.85) and excellent (AUC — 0.9) prediction accuracy, respectively. This study tested new techniques to identify threshold values of predictors, providing for their classification as HM risk factors and ensuring clinical justification for the prognosis results.
Zhu et al. [39] on a cohort of 5836 patients with STEMI and NSTEMI after PCI (3587 — training sample, 1196 — test sample, 1053 — validation sample) used 7 ML techniques to develop HM models with excellent prediction accuracy. The model based on an ensemble meta-algorithm (Bagging) had the highest accuracy (AUC — 0.932) and included 8 predictors, where D-dimer, BNP, and blood phosphorus concentration have not been previously used in the analyzed algorithms. It is noteworthy that D-dimer and BNP had the greatest impact on HM, and the impact of neutrophils and prothrombin index to the end point was comparable to the cardiogenic shock factor.
Discussion
In recent years, predictive analysis techniques have been widely used in clinical medicine, which is confirmed by the constantly growing number of scientific researches on the issue [69–80]. This approach is of particular relevance in life-threatening conditions, including STEMI. The systematic review provides an analysis of publications showing the evolution of HM prediction techniques in STEMI over the past 25 years. The majority of the “classical” scales were developed and validated on large samples of patients in the first decade of this century (see Table 1). At that, 3 of them (PREDICT, GRACE, RECORD) were developed based on data from the similarly called registries of patients with ACS, and 5 scales (GUSTO, TIMI risk score for STEMI, Zwolle, PAMI, and CADILLAC) — based on data from registries of patients with STEMI. The structure of the majority of the analyzed scales included HM predictors, which were considered referential (age of patients, AHF class (T. Killip class), HR, and SBP). The CADILLAC and Zwolle scales also include TVCAD and TIMI indicators, which are associated with a more accurate stratification of HM risk after PCI. Laboratory indicators Cr, GFR, Ht, and Hb add up to the list of predictors in the PREDICT, CADILLAC, GRACE, and RECORD scales, and LVEF indicators and time to myocardial revascularization >4 h — in the TIMI risk score for STEMI and Zwolle scales. According to the AUC values classifier [81], only the Zwolle scale had excellent predictive accuracy (AUC≥0.9), the GRACE, CADILLAC, GUSTO, and RECORD scales have appropriate predictive accuracy (0.8≤AUC<0.9), whereas PREDICT, TIMI risk score for STEMI and PAMI have acceptable predictive accuracy (0.7≤AUC<0.8). It is known that the best quality of predictive models is most often demonstrated in the populations from which the original data were received [82]. At that, many studies demonstrated that the GRACE and CADILLAC scales used on external samples had higher predictive accuracy than other classical scales [83, 84]. It should be noted that all analyzed scales were developed using the following basic ML techniques: MLR and CR. Their advantage is the transparency of predictive decisions, and the disadvantage relates to considering only linear relations between predictors and the end point of the study, which limits their predictive potential.
|
Table 1. Analysis of the predictive accuracy of classical models of hospital mortality in patients with STEMI |
Currently, an active search for new predictors of STEMI-associated adverse events is ongoing. In various publications, newly identified HM predictors for this category of patients are related to signs of comorbidity, clinical, biochemical, and hematological indicators of inflammatory response, metabolic status parameters, heart chamber volumes, atrial fibrillation, BNP, D-dimer, and etc. Due to the prevailing strategy of myocardial revascularization by means of PCI, the need to develop HM risk measurement tools after PCI is growing. According to literature, fatal outcomes after emergency PCI are recorded in 4–7% of patients with STEMI, which makes the issue of HM risk stratification relevant [62]. HM predictors after PCI most often include signs of failure according to TIMI — 0–2 (slow-reflow and no-reflow phenomena), criteria of coronary lesions according to SS I or SS II, hemodynamic parameters, blood glucose levels, and etc. [85–98].
To increase the information value of predictors and develop interpretable ML models, explainable artificial intelligence techniques have been used in recent years. These techniques include identification of predictors’ threshold values, deviation from which increases their predictive value and allows their classification as risk factors for adverse events [67]. A new approach in ML model development is phenotyping of risk factors and ranking of specific predictors per the intensity of their influence on the end point of the study [26, 99–102]. The analysis of recent publications demonstrated that the majority of the current predictive models were developed using modern ML techniques (RF, SVM, DT, SGB, ANN, ensembles of models), which in most cases have appropriate or excellent accuracy (see Table 2). Their advantage is the ability to identify hidden or non-obvious patterns, as well as to get new knowledge from big data. An important area of risk measurement in STEMI is still the development of HM prognostic models for patients in the ICU due to the disease complications. The review mentions publications with examples of such algorithms, the predictors of which include invasive indicators of cardiohemodynamics, indicators of oxygen delivery and consumption, blood lactate concentration, administration of vasoactive drugs, and etc. These models were superior in accuracy to classical emergency risk scales (APACHE II, SAPS, SI) [40–43].
|
Table 2. Analysis of prognostic accuracy of new hospital mortality risk measurement tools in patients with STEMI |
Conclusion
The analysis of scientific literature points to a growing interest of researchers in improvement of prognostic technologies that provide reliable risk stratification of hospital mortality in STEMI. This issue is associated with development of interpretable ML models that can explain generated conclusions, which contributed to building trust of doctors. Here, an important task is implementation of prognostic models of adverse events in medical decision support systems, which provide additional information required to assess the risks of hospital mortality in daily clinical practice. A necessary condition for evolution of prognostic technologies for hospital mortality is also development and constant update of regional and national registers of patients with STEMI, which take into account specifics of resource support for cardiological service.
Author contributions: B.I. Geltser proposed the concept of the study, managed the research and preparation of the manuscript; I.G. Domzhalov, E.A. Kokarev, R.L. Pak were responsible for data collection and result interpretation; K.I. Shakhgeldyan developed the study design; N.S. Kuksin, V.N. Kotelnikov analyzed the data and prepared the text of the publication.
Financing. The research was performed within the framework of project FZNS-2023-0010 State Assignments to the Far Eastern Federal University.
Conflict of interest. The authors declare no conflict of interest.
References
- Alekyan B.G., Boytsov S.A., Manoshkina E.M., Ganyukov V.I. Myocardial revascularization in Russian Federation for acute coronary syndrome in 2016–2020. Kardiologiia 2021; 61(12): 4–15, https://doi.org/10.18087/cardio.2021.12.n1879.
- Grabowski M., Filipiak K.J., Opolski G., Glowczynska R. How to improve prognostic value of popular risk scores used in acute coronary syndrome — a single center experience in a long term follow-up. Curr Res Cardiol 2018; 5(3): 30–33, https://doi.org/10.4172/2368-0512.1000108.
- Fox K.A., Dabbous O.H., Goldberg R.J., Pieper K.S., Eagle K.A., Van de Werf F., Avezum A., Goodman S.G., Flather M.D., Anderson F.A. Jr, Granger C.B. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 2006; 333(7578): 1091, https://doi.org/10.1136/bmj.38985.646481.55.
- Halkin A., Singh M., Nikolsky E., Grines C.L., Tcheng J.E., Garcia E., Cox D.A., Turco M., Stuckey T.D., Na Y., Lansky A.J., Gersh B.J., O’Neill W.W., Mehran R., Stone G.W. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol 2005; 45(9): 1397–1405, https://doi.org/10.1016/j.jacc.2005.01.041.
- Morrow D.A., Antman E.M., Charlesworth A., Cairns R., Murphy S.A., de Lemos J.A., Giugliano R.P., McCabe C.H., Braunwald E. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000; 102(17): 2031–2037, https://doi.org/10.1161/01.cir.102.17.2031.
- Erlikh A.D. A scale for early assessment of risk of death or myocardial infarction during initial hospitalization of patients with acute coronary syndromes (based on data from the RECORD registry). Kardiologiia 2010; 10: 11–16.
- Jacobs D.R. Jr, Kroenke C., Crow R., Deshpande M., Gu D.F., Gatewood L., Blackburn H. PREDICT: a simple risk score for clinical severity and long-term prognosis after hospitalization for acute myocardial infarction or unstable angina: the Minnesota heart survey. Circulation 1999; 100(6): 599–607, https://doi.org/10.1161/01.cir.100.6.599.
- Califf R.M., Pieper K.S., Lee K.L., Van De Werf F., Simes R.J., Armstrong P.W., Topol E.J. Prediction of 1-year survival after thrombolysis for acute myocardial infarction in the global utilization of streptokinase and TPA for occluded coronary arteries trial. Circulation 2000; 101(19): 2231–2238, https://doi.org/10.1161/01.cir.101.19.2231.
- Addala S., Grines C.L., Dixon S.R., Stone G.W., Boura J.A., Ochoa A.B., Pellizzon G., O’Neill W.W., Kahn J.K. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI risk score). Am J Cardiol 2004; 93(5): 629–632, https://doi.org/10.1016/j.amjcard.2003.11.036.
- De Luca G., Suryapranata H., van’t Hof A.W., de Boer M.J., Hoorntje J.C., Dambrink J.H., Gosselink A.T., Ottervanger J.P., Zijlstra F. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation 2004; 109(22): 2737–2743, https://doi.org/10.1161/01.CIR.0000131765.73959.87.
- Fox K.A., Fitzgerald G., Puymirat E., Huang W., Carruthers K., Simon T., Coste P., Monsegu J., Gabriel Steg P., Danchin N., Anderson F. Should patients with acute coronary disease be stratified for management according to their risk? Derivation, external validation and outcomes using the updated GRACE risk score. BMJ Open 2014; 4(2): e004425, https://doi.org/10.1136/bmjopen-2013-004425.
- Szabo D., Szabo A., Magyar L., Banhegyi G., Kugler S., Pinter A., Juhasz V., Ruppert M., Olah A., Ruzsa Z., Edes I.F., Szekely A., Becker D., Merkely B., Hizoh I. Admission lactate level and the GRACE 2.0 score are independent and additive predictors of 30-day mortality of STEMI patients treated with primary PCI-results of a real-world registry. PLoS One 2022; 17(11): e0277785, https://doi.org/10.1371/journal.pone.0277785.
- Xiao L., Jia Y., Wang X., Huang H. The impact of preoperative fibrinogen-albumin ratio on mortality in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Clin Chim Acta 2019; 493: 8–13, https://doi.org/10.1016/j.cca.2019.02.018.
- Klingenberg R., Aghlmandi S., Räber L., Gencer B., Nanchen D., Heg D., Carballo S., Rodondi N., Mach F., Windecker S., Jüni P., von Eckardstein A., Matter C.M., Lüscher T.F. Improved risk stratification of patients with acute coronary syndromes using a combination of hsTnT, NT-proBNP and hsCRP with the GRACE score. Eur Heart J Acute Cardiovasc Care 2018; 7(2): 129–138, https://doi.org/10.1177/2048872616684678.
- Xiong S., Chen Q., Chen X., Hou J., Chen Y., Long Y., Yang S., Qi L., Su H., Huang W., Liu H., Zhang Z., Cai L. Adjustment of the GRACE score by the triglyceride glucose index improves the prediction of clinical outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Cardiovasc Diabetol 2022; 21(1): 145, https://doi.org/10.1186/s12933-022-01582-w.
- Pang S., Miao G., Zhou Y., Du Y., Rui Z., Zhao X. Addition of TyG index to the GRACE score improves prediction of adverse cardiovascular outcomes in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: a retrospective study. Front Cardiovasc Med 2022; 9: 957626, https://doi.org/10.3389/fcvm.2022.957626.
- Li Q., Ma X., Shao Q., Yang Z., Wang Y., Gao F., Zhou Y., Yang L., Wang Z. Prognostic impact of multiple lymphocyte-based inflammatory indices in acute coronary syndrome patients. Front Cardiovasc Med 2022; 9: 811790, https://doi.org/10.3389/fcvm.2022.811790.
- Dalimunthe N.N., Alwi I., Nasution S.A., Shatri H. The role of Tei index added to the GRACE risk score for prediction of in-hospital MACE after acute myocardial infarction. Rom J Intern Med 2022; 60(4): 222–228, https://doi.org/10.2478/rjim-2022-0012.
- Xiong S., Luo Y., Chen Q., Chen Y., Su H., Long Y., Chen X., Yang S., Qi L., Huang W., Hou J., Liu H., Cai L. Adjustment of the GRACE score by the stress hyperglycemia ratio improves the prediction of long-term major adverse cardiac events in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a multicenter retrospective study. Diabetes Res Clin Pract 2023; 198: 110601, https://doi.org/10.1016/j.diabres.2023.110601.
- Chen X., Xiong S., Chen Y., Cheng L., Chen Q., Yang S., Qi L., Liu H., Cai L. The predictive value of different nutritional indices combined with the GRACE score in predicting the risk of long-term death in patients with acute coronary syndrome undergoing percutaneous coronary intervention. J Cardiovasc Dev Dis 2022; 9(10): 358, https://doi.org/10.3390/jcdd9100358.
- Liu X.J., Wan Z.F., Zhao N., Zhang Y.P., Mi L., Wang X.H., Zhou D., Wu Y., Yuan Z.Y. Adjustment of the GRACE score by hemoglobinA1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol 2015; 14: 110, https://doi.org/10.1186/s12933-015-0274-4.
- Zhang S., Wan Z., Zhang Y., Fan Y., Gu W., Li F., Meng L., Zeng X., Han D., Li X. Neutrophil count improves the GRACE risk score prediction of clinical outcomes in patients with ST-elevation myocardial infarction. Atherosclerosis 2015; 241(2): 723–728, https://doi.org/10.1016/j.atherosclerosis.2015.06.035.
- Chen Q., Su H., Yu X., Chen Y., Ding X., Xiong B., Wang C., Xia L., Ye T., Lan K., Hou J., Xiong S., Cai L. The stress hyperglycemia ratio improves the predictive ability of the GRACE score for in-hospital mortality in patients with acute myocardial infarction. Hellenic J Cardiol 2023; 70: 36–45, https://doi.org/10.1016/j.hjc.2022.12.012.
- Geltser B.I., Shahgeldyan K.I., Domzhalov I.G., Kuksin N.S., Kokarev E.A., Kotelnikov V.N., Rublev V.Yu. Prediction of in-hospital mortality in patients with ST-segment elevation acute myocardial infarction after percutaneous coronary intervention. Russian Journal of Cardiology 2023; 28(6): 5414, https://doi.org/10.15829/1560-4071-2023-5414.
- Erlikh A.D. Opportunity to select patients for primary invasive intervention in ACS with ST-segment elevation using “RECORD” modified scale. Trudnyy patsient 2013; 11(7): 36–39.
- Shakhgeldyan K.I., Kuksin N.S., Domzhalov I.G., Rublev V.Y., Geltser B.I. Interpretable machine learning for in-hospital mortality risk prediction in patients with ST-elevation myocardial infarction after percutaneous coronary interventions. Comput Biol Med 2024; 170: 107953, https://doi.org/10.1016/j.compbiomed.2024.107953.
- Farooq V., van Klaveren D., Steyerberg E.W., Meliga E., Vergouwe Y., Chieffo A., Kappetein A.P., Colombo A., Holmes D.R. Jr, Mack M., Feldman T., Morice M.C., Ståhle E., Onuma Y., Morel M.A., Garcia-Garcia H.M., van Es G.A., Dawkins K.D., Mohr F.W., Serruys P.W. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 2013; 381(9867): 639–650, https://doi.org/10.1016/S0140-6736(13)60108-7.
- Karabağ Y., Çağdaş M., Rencuzogullari I., Karakoyun S., Artaç İ., İliş D., Yesin M., Öterkus M., Gokdeniz T., Burak C., Tanboğa I.H. Comparison of SYNTAX score II efficacy with SYNTAX score and TIMI risk score for predicting in-hospital and long-term mortality in patients with ST segment elevation myocardial infarction. Int J Cardiovasc Imaging 2018; 34(8): 1165–1175, https://doi.org/10.1007/s10554-018-1333-1.
- McNamara R.L., Kennedy K.F., Cohen D.J., Diercks D.B., Moscucci M., Ramee S., Wang T.Y., Connolly T., Spertus J.A. Predicting in-hospital mortality in patients with acute myocardial infarction. J Am Coll Cardiol 2016; 68(6): 626–635, https://doi.org/10.1016/j.jacc.2016.05.049.
- Rodríguez-Jiménez A.E., Negrín-Valdés T., Cruz-Inerarity H., Castellano-Gallo L.A., Chávez-González E. Prognostic scale to stratify risk of intrahospital death in patients with acute myocardial infarction with ST-segment elevation. MEDICC Rev 2020; 22(3): 46–53, https://doi.org/10.37757/MR2020.V22.N3.10.
- Bessonov I.S., Kuznetsov V.A., Sapozhnikov S.S., Gorbatenko E.A., Shadrin A.A. The risk score for in-hospital mortality in patients with ST-segment elevation myocardial infarction. Kardiologiia 2021; 61(9): 11–19, https://doi.org/10.18087/cardio.2021.9.n1720.
- Hadanny A., Shouval R., Wu J., Shlomo N., Unger R., Zahger D., Matetzky S., Goldenberg I., Beigel R., Gale C., Iakobishvili Z. Predicting 30-day mortality after ST elevation myocardial infarction: machine learning-based random forest and its external validation using two independent nationwide datasets. J Cardiol 2021; 78(5): 439–446, https://doi.org/10.1016/j.jjcc.2021.06.002.
- Millo L., McKenzie A., De la Paz A., Zhou C., Yeung M., Stouffer G.A. Usefulness of a novel risk score to predict in-hospital mortality in patients ≥60 years of age with ST elevation myocardial infarction. Am J Cardiol 2021; 154: 1–6, https://doi.org/10.1016/j.amjcard.2021.05.036.
- Tan L., Xu Q., Shi R. A nomogram for predicting hospital mortality in intensive care unit patients with acute myocardial infarction. Int J Gen Med 2021; 14: 5863–5877, https://doi.org/10.2147/IJGM.S326898.
- Jain A., Fong H.K., Ijaz H.M., Desai R. Predictors of in-hospital mortality in young adults hospitalized with ST-elevation myocardial infarction: an artificial neural network analysis using a nationwide cohort. J Am Coll Cardiol 2022; 79(9): 1064, https://doi.org/10.1016/s0735-1097(22)02055-1.
- Deng L., Zhao X., Su X., Zhou M., Huang D., Zeng X. Machine learning to predict no reflow and in-hospital mortality in patients with ST-segment elevation myocardial infarction that underwent primary percutaneous coronary intervention. BMC Med Inform Decis Mak 2022; 22(1): 109, https://doi.org/10.1186/s12911-022-01853-2.
- Zhao P., Liu C., Zhang C., Hou Y., Zhang X., Zhao J., Sun G., Zhou J. Using machine learning to predict the in-hospital mortality in women with ST-segment elevation myocardial infarction. Rev Cardiovasc Med 2023, 24(5): 126, https://doi.org/10.31083/j.rcm2405126.
- Li R., Shen L., Ma W., Yan B., Chen W., Zhu J., Li L., Yuan J., Pan C. Use of machine learning models to predict in-hospital mortality in patients with acute coronary syndrome. Clin Cardiol 2023; 46(2): 184–194, https://doi.org/10.1002/clc.23957.
- Zhu X., Xie B., Chen Y., Zeng H., Hu J. Machine learning in the prediction of in-hospital mortality in patients with first acute myocardial infarction. Clin Chim Acta 2024; 554: 117776, https://doi.org/10.1016/j.cca.2024.117776.
- Norton J.M., Reddy P.K., Subedi K., Fabrizio C.A., Wimmer N.J., Urrutia L.E. Utilization of an ICU severity of illness scoring system to triage patients with ST-elevation myocardial infarction. J Intensive Care Med 2021; 36(8): 857–861, https://doi.org/10.1177/0885066620928263.
- Guo C., Luo X.L., Gao X.J., Wang J., Liu R., Li J., Zhang J., Yang W.X., Hu F.H., Wu Y., Yang Y.J., Qiao S.B. Comparison on the predictive value of different scoring systems for risk of short-term death in patients with acute myocardial infarction complicating cardiogenic shock. Zhonghua Xin Xue Guan Bing Za Zhi 2018; 46(7): 529–535, https://doi.org/10.3760/cma.j.issn.0253-3758.2018.07.005.
- Chiang C.Y., Lin C.F., Liu P.H., Chen F.C., Chiu I.M., Cheng F.J. Clinical validation of the shock index, modified shock index, delta shock index, and shock index-C for emergency department ST-segment elevation myocardial infarction. J Clin Med 2022; 11(19): 5839, https://doi.org/10.3390/jcm11195839.
- Wang S., Zhang Y., Cheng Q., Qi D., Wang X., Zhu Z., Li M., Zhang J., Hu D., Gao C. Shock index-based risk indices as prognostic predictor for in-hospital mortality in patients with ST-elevation myocardial infarction, the results from Henan STEMI registry. Preprint (Version 1) 2022 Apr 11, https://doi.org/10.21203/rs.3.rs-1512785/v1.
- Li F., Li D., Yu J., Jia Y., Jiang Y., Chen X., Gao Y., Ye L., Wan Z., Cao Y., Zeng Z., Zeng R. Prognostic value of the Nutritional Risk Screening 2002 Scale in patients with acute myocardial infarction: insights from the retrospective multicenter study for early evaluation of acute chest pain. J Cardiovasc Nurs 2021; 36(6): 546–555, https://doi.org/10.1097/JCN.0000000000000786.
- Jia Y., Li H., Li D., Li F., Li Q., Jiang Y., Gao Y., Wan Z., Cao Y., Zeng Z., Zeng R. Prognostic value of Braden Scale in patients with acute myocardial infarction: from the retrospective multicenter study for early evaluation of acute chest pain. J Cardiovasc Nurs 2020; 35(6): E53–E61, https://doi.org/10.1097/JCN.0000000000000735.
- Ndrepepa G., Holdenrieder S., Kastrati A. Prognostic value of De Ritis ratio in patients with acute myocardial infarction. Clin Chim Acta 2022; 535: 75–81, https://doi.org/10.1016/j.cca.2022.08.016.
- Rivera-Fernández R., Arias-Verdú M.D., García-Paredes T., Delgado-Rodríguez M., Arboleda-Sánchez J.A., Aguilar-Alonso E., Quesada-García G., Vera-Almazán A. Prolonged QT interval in ST-elevation myocardial infarction and mortality: new prognostic scale with QT, Killip and age. J Cardiovasc Med (Hagerstown) 2016; 17(1): 11–19, https://doi.org/10.2459/JCM.0000000000000015.
- Kwon J.M., Jeon K.H., Kim H.M., Kim M.J., Lim S., Kim K.H., Song P.S., Park J., Choi R.K., Oh B.H. Deep-learning-based risk stratification for mortality of patients with acute myocardial infarction. PLoS One 2019; 14(10): e0224502, https://doi.org/10.1371/journal.pone.0224502.
- Sherazi S.W.A., Zheng H., Lee J.Y. A machine learning-based applied prediction model for identification of acute coronary syndrome (ACS) outcomes and mortality in patients during the hospital stay. Sensors (Basel) 2023; 23(3): 1351, https://doi.org/10.3390/s23031351.
- Kasim S., Malek S., Song C., Wan Ahmad W.A., Fong A., Ibrahim K.S., Safiruz M.S., Aziz F., Hiew J.H., Ibrahim N. In-hospital mortality risk stratification of Asian ACS patients with artificial intelligence algorithm. PLoS One 2022; 17(12): e0278944, https://doi.org/10.1371/journal.pone.0278944.
- Singh A., Miller R.J.H., Otaki Y., Kavanagh P., Hauser M.T., Tzolos E., Kwiecinski J., Van Kriekinge S., Wei C.C., Sharir T., Einstein A.J., Fish M.B., Ruddy T.D., Kaufmann P.A., Sinusas A.J., Miller E.J., Bateman T.M., Dorbala S., Di Carli M., Liang J.X., Huang C., Han D., Dey D., Berman D.S., Slomka P.J. Direct risk assessment from myocardial perfusion imaging using explainable deep learning. JACC Cardiovasc Imaging 2023; 16(2): 209–220, https://doi.org/10.1016/j.jcmg.2022.07.017.
- Hizoh I., Banhegyi G., Domokos D., Major L., Andrassy P., Andreka P., Becker D., Buttl A., Cziraki A., Dezsi C.A., Edes I., Forster T., Herczeg B., Janosi A., Katona A., Kiss R., Koszegi Z., Lupkovics G., Nagy G., Nagy L., Noori E., Tomcsanyi J., Veress G., Ruzsa Z., Merkely B. TCT-804 comparative validation of the ALPHA score, a novel risk model including vascular access site for predicting 30-day mortality in patients treated with primary PCI. J Am Coll Cardiol 2018; 72 (13 Suppl): B320–B321, https://doi.org/10.1016/j.jacc.2018.08.2039.
- Hizoh I., Domokos D., Banhegyi G., Becker D., Merkely B., Ruzsa Z. Mortality prediction algorithms for patients undergoing primary percutaneous coronary intervention. J Thorac Dis 2020; 12(4): 1706–1720, https://doi.org/10.21037/jtd.2019.12.83.
- Zhang X.T., Lin Z.R., Zhang L., Zhao Z.W., Chen L.L. MELD-XI score predict no-reflow phenomenon and short-term mortality in patient with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. BMC Cardiovasc Disord 2022; 22(1): 113, https://doi.org/10.1186/s12872-022-02556-2.
- Toprak K., Toprak İ.H., Acar O., Ermiş M.F. The predictive value of the HALP score for no-reflow phenomenon and short-term mortality in patients with ST-elevation myocardial infarction. Postgrad Med 2024; 136(2): 169–179, https://doi.org/10.1080/00325481.2024.2319567.
- Safak O., Yildirim T., Emren V., Avci E., Argan O., Aktas Z., Yildirim S.E., Akgun D.E., Kisacik H.L. Prognostic nutritional index as a predictor of no-reflow occurrence in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention. Angiology 2024; 75(7): 689–695, https://doi.org/10.1177/00033197231193223.
- Kumar R., Ahmed I., Rai L., Khowaja S., Hashim M., Huma Z., Sial J.A., Saghir T., Qamar N., Karim M. Comparative analysis of four established risk scores for prediction of in-hospital mortality in patients undergoing primary percutaneous coronary intervention. Am J Cardiovasc Dis 2022; 12(6): 298–306.
- Sivkov O.G. Factors associated with hospital mortality in acute myocardial infarction. Kardiologiia 2023; 63(11): 29–35, https://doi.org/10.18087/cardio.2023.11.n2406.
- Semaan C., Charbonnier A., Pasco J., Darwiche W., Saint Etienne C., Bailleul X., Bourguignon T., Fauchier L., Angoulvant D., Ivanes F., Genet T. Risk scores in ST-segment elevation myocardial infarction patients with refractory cardiogenic shock and veno-arterial extracorporeal membrane oxygenation. J Clin Med 2021; 10(5): 956, https://doi.org/10.3390/jcm10050956.
- Reindl M., Reinstadler S.J., Tiller C., Kofler M., Theurl M., Klier N., Fleischmann K., Mayr A., Henninger B., Klug G., Metzler B. ACEF score adapted to ST-elevation myocardial infarction patients: the ACEF-STEMI score. Int J Cardiol 2018; 264: 18–24, https://doi.org/10.1016/j.ijcard.2018.04.017.
- Sevdımbas S., Satar S., Gulen M., Acehan S., Acele A., Koksaldı Sahin G., Aka Satar D. Blood urea nitrogen/albumin ratio on admission predicts mortality in patients with non ST segment elevation myocardial infarction. Scand J Clin Lab Invest 2022; 82(6): 454–460, https://doi.org/10.1080/00365513.2022.2122075.
- Geltser B.I., Rublev V.Yu., Tsivanyuk M.M., Shakhgeldyan K.I. Machine learning in predicting immediate and long-term outcomes of myocardial revascularization: a systematic review. Russian Journal of Cardiology 2021; 26(8): 4505, https://doi.org/10.15829/1560-4071-2021-4505.
- Chen P., Wang B., Zhao L., Ma S., Wang Y., Zhu Y., Zeng X., Bai Z., Shi B. Machine learning for predicting intrahospital mortality in ST-elevation myocardial infarction patients with type 2 diabetes mellitus. BMC Cardiovasc Disord 2023; 23(1): 585, https://doi.org/10.1186/s12872-023-03626-9.
- Xiao C., Guo Y., Zhao K., Liu S., He N., He Y., Guo S., Chen Z. Prognostic value of machine learning in patients with acute myocardial infarction. J Cardiovasc Dev Dis 2022; 9(2): 56, https://doi.org/10.3390/jcdd9020056.
- D’Ascenzo F., De Filippo O., Gallone G., Mittone G., Deriu M.A., Iannaccone M., Ariza-Solé A., Liebetrau C., Manzano-Fernández S., Quadri G., Kinnaird T., Campo G., Simao Henriques J.P., Hughes J.M., Dominguez-Rodriguez A., Aldinucci M., Morbiducci U., Patti G., Raposeiras-Roubin S., Abu-Assi E., De Ferrari G.M.; PRAISE study group. Machine learning-based prediction of adverse events following an acute coronary syndrome (PRAISE): a modelling study of pooled datasets. Lancet 2021; 397(10270): 199–207, https://doi.org/10.1016/S0140-6736(20)32519-8.
- Zhao J., Zhao P., Li C., Hou Y. Optimized machine learning models to predict in-hospital mortality for patients with ST-segment elevation myocardial infarction. Ther Clin Risk Manag 2021; 17: 951–961, https://doi.org/10.2147/TCRM.S321799.
- Shakhgeldyan K.I., Geltser B.I., Kuksin N.S., Domzhalov I.G. Multilevel categorization of continuous variables in the tasks of explaining predictive estimates of machine learning models in clinical medicine. Vrach i informatsionnye tekhnologii 2023; 3: 44–57, https://doi.org/10.25881/18110193_2023_3_44.
- Ong A.T., Serruys P.W., Mohr F.W., Morice M.C., Kappetein A.P., Holmes D.R. Jr, Mack M.J., van den Brand M., Morel M.A., van Es G.A., Kleijne J., Koglin J., Russell M.E. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J 2006; 151(6): 1194–1204, https://doi.org/10.1016/j.ahj.2005.07.017.
- Lee S., Chu Y., Ryu J., Park Y.J., Yang S., Koh S.B. Artificial intelligence for detection of cardiovascular-related diseases from wearable devices: a systematic review and meta-analysis. Yonsei Med J 2022; 63(Suppl): S93–S107, https://doi.org/10.3349/ymj.2022.63.S93.
- Popat A., Yadav S., Patel S.K., Baddevolu S., Adusumilli S., Rao Dasari N., Sundarasetty M., Anand S., Sankar J., Jagtap Y.G. Artificial intelligence in the early prediction of cardiogenic shock in acute heart failure or myocardial infarction patients: a systematic review and meta-analysis. Cureus 2023; 15(12): e50395, https://doi.org/10.7759/cureus.50395.
- Zhang Z., Zhao Y., Canes A., Steinberg D., Lyashevska O.; written on behalf of AME Big-Data Clinical Trial Collaborative Group. Predictive analytics with gradient boosting in clinical medicine. Ann Transl Med 2019; 7(7): 152, https://doi.org/10.21037/atm.2019.03.29.
- Wu Y., Chen H., Li L., Zhang L., Dai K., Wen T., Peng J., Peng X., Zheng Z., Jiang T., Xiong W. Construction of novel gene signature-based predictive model for the diagnosis of acute myocardial infarction by combining random forest with artificial neural network. Front Cardiovasc Med 2022; 9: 876543, https://doi.org/10.3389/fcvm.2022.876543.
- Chang Y., Antonescu C., Ravindranath S., Dong J., Lu M., Vicario F., Wondrely L., Thompson P., Swearingen D., Acharya D. Early prediction of cardiogenic shock using machine learning. Front Cardiovasc Med 2022; 9: 862424, https://doi.org/10.3389/fcvm.2022.862424.
- Gong M., Liang D., Xu D., Jin Y., Wang G., Shan P. Analyzing predictors of in-hospital mortality in patients with acute ST-segment elevation myocardial infarction using an evolved machine learning approach. Comput Biol Med 2024; 170: 107950, https://doi.org/10.1016/j.compbiomed.2024.107950.
- Oliveira M., Seringa J., Pinto F.J., Henriques R., Magalhães T. Machine learning prediction of mortality in acute myocardial infarction. BMC Med Inform Decis Mak 2023; 23(1): 70, https://doi.org/10.1186/s12911-023-02168-6.
- Khera R., Haimovich J., Hurley N.C., McNamara R., Spertus J.A., Desai N., Rumsfeld J.S., Masoudi F.A., Huang C., Normand S.L., Mortazavi B.J., Krumholz H.M. Use of machine learning models to predict death after acute myocardial infarction. JAMA Cardiol 2021; 6(6): 633–641, https://doi.org/10.1001/jamacardio.2021.0122.
- Lee H.C., Park J.S., Choe J.C., Ahn J.H., Lee H.W., Oh J.H., Choi J.H., Cha K.S., Hong T.J., Jeong M.H.; Korea Acute Myocardial Infarction Registry (KAMIR) and Korea Working Group on Myocardial Infarction (KorMI) Investigators. Prediction of 1-year mortality from acute myocardial infarction using machine learning. Am J Cardiol 2020; 133: 23–31, https://doi.org/10.1016/j.amjcard.2020.07.048.
- Aziz F., Malek S., Ibrahim K.S., Raja Shariff R.E., Wan Ahmad W.A., Ali R.M., Liu K.T., Selvaraj G., Kasim S. Short- and long-term mortality prediction after an acute ST-elevation myocardial infarction (STEMI) in Asians: a machine learning approach. PLoS One 2021; 16(8): e0254894, https://doi.org/10.1371/journal.pone.0254894.
- Liu R., Wang M., Zheng T., Zhang R., Li N., Chen Z., Yan H., Shi Q. An artificial intelligence-based risk prediction model of myocardial infarction. BMC Bioinformatics 2022; 23(1): 217, https://doi.org/10.1186/s12859-022-04761-4.
- Tarabanis C., Kalampokis E., Khalil M., Alviar C.L., Chinitz L.A., Jankelson L. Explainable SHAP-XGBoost models for in-hospital mortality after myocardial infarction. Cardiovasc Digit Health J 2023; 4(4): 126–132, https://doi.org/10.1016/j.cvdhj.2023.06.001.
- Hosmer D.W. Jr, Lemeshow S., Sturdivant R.X. Applied logistic regression, 3rd edition: guide to logistic regression modeling. John Wiley & Sons, Inc; 2013; 177 p.
- Alizadehsani R., Abdar M., Roshanzamir M., Khosravi A., Kebria P.M., Khozeimeh F., Nahavandi S., Sarrafzadegan N., Acharya U.R. Machine learning-based coronary artery disease diagnosis: a comprehensive review. Comput Biol Med 2019; 111: 103346, https://doi.org/10.1016/j.compbiomed.2019.103346.
- Wang C.H., Wang H.T., Wu K.H., Cheng F.J., Cheng C.I., Kung C.T., Chen F.C. Comparison of different risk scores for prediction of in-hospital mortality in STEMI patients treated with PPCI. Emerg Med Int 2022; 2022: 5389072, https://doi.org/10.1155/2022/5389072.
- Ji C., Song F., Huang X., Qu X., Qiu N., Zhu J. Comparison of the predictive value of the modified CADILLAC, GRACE and TIMI risk scores for the risk of short-term death in patients with acute ST segment elevation myocardial infarction after percutaneous coronary intervention. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2023; 35(3): 299–304, https://doi.org/10.3760/cma.j.cn121430-20220727-00696.
- Ali M., Lange S.A., Wittlinger T., Lehnert G., Rigopoulos A.G., Noutsias M. In-hospital mortality after acute STEMI in patients undergoing primary PCI. Herz 2018; 43(8): 741–745, https://doi.org/10.1007/s00059-017-4621-y.
- Kocas B.B., Cetinkal G., Kocas C., Arslan S., Abaci O., Dalgic Y., Ser O.S., Batit S., Yildiz A., Dogan S.M. Usefulness of the SYNTAX score II to predict in-hospital and long-term mortality in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Sisli Etfal Hastan Tip Bul 2022; 56(2): 182–188, https://doi.org/10.14744/SEMB.2021.33410.
- Saygi M., Tanalp A.C., Tezen O., Pay L., Dogan R., Uzman O., Karabay C.Y., Tanboga I.H., Kacar F.O., Karagoz A. The prognostic importance of the Naples prognostic score for in-hospital mortality in patients with ST-segment elevation myocardial infarction. Coron Artery Dis 2024; 35(1): 31–37, https://doi.org/10.1097/MCA.0000000000001285.
- Szabó G.T., Ágoston A., Csató G., Rácz I., Bárány T., Uzonyi G., Szokol M., Sármán B., Jebelovszki É., Édes I.F., Czuriga D., Kolozsvári R., Csanádi Z., Édes I., Kőszegi Z. Predictors of hospital mortality in patients with acute coronary syndrome complicated by cardiogenic shock. Sensors (Basel) 2021; 21(3): 969, https://doi.org/10.3390/s21030969.
- El Farissi M., Zimmermann F.M., De Maria G.L., van Royen N., van Leeuwen M.A.H., Carrick D., Carberry J., Wijnbergen I.F., Konijnenberg L.S.F., Hoole S.P., Marin F., Fineschi M., Pijls N.H.J., Oldroyd K.G., Banning A.P., Berry C., Fearon W.F. The index of microcirculatory resistance after primary PCI: a pooled analysis of individual patient data. JACC Cardiovasc Interv 2023; 16(19): 2383–2392, https://doi.org/10.1016/j.jcin.2023.08.030.
- Lu X., Lin X., Cai Y., Zhang X., Meng H., Chen W., Yu P., Chen X. Association of the triglyceride-glucose index with severity of coronary stenosis and in-hospital mortality in patients with acute ST elevation myocardial infarction after percutaneous coronary intervention: a multicentre retrospective analysis cohort study. BMJ Open 2024; 14(3): e081727, https://doi.org/10.1136/bmjopen-2023-081727.
- Huang L., Zhang J., Huang Q., Cui R., Chen J. In-hospital major adverse cardiovascular events after primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction: a retrospective study under the China chest pain center (standard center) treatment system. BMC Cardiovasc Disord 2023; 23(1): 198, https://doi.org/10.1186/s12872-023-03214-x.
- Vatan M.B., Çakmak A.C., Ağaç S., Eynel E., Erkan H. The systemic immune-inflammation index predicts impaired myocardial perfusion and short-term mortality in ST-segment elevation myocardial infarction patients. Angiology 2023; 74(4): 365–373, https://doi.org/10.1177/00033197221106886.
- Kim K., Kang M.G., Park H.W., Koh J.S., Park J.R., Hwang S.J., Hwang J.Y. Prognostic utility of culprit SYNTAX score in patients with cardiogenic shock complicating ST-segment elevation myocardial infarction. Am J Cardiol 2021; 154: 14–21, https://doi.org/10.1016/j.amjcard.2021.05.035.
- Biccirè F.G., Farcomeni A., Gaudio C., Pignatelli P., Tanzilli G., Pastori D. D-dimer for risk stratification and antithrombotic treatment management in acute coronary syndrome patients: asystematic review and metanalysis. Thromb J 2021; 19(1): 102, https://doi.org/10.1186/s12959-021-00354-y.
- Bessonov I.S., Sapozhnikov S.S., Shadrin A.A., Kashtanov M.G., Popov S.V. Effect of the “door-to-balloon” time on the results of treatment of patients with ST-segment elevation myocardial infarction, depending on the duration of the pre-hospital delay. Kardiologiia 2023; 63(6): 28–36, https://doi.org/10.18087/cardio.2023.6.n2245.
- Wang K., Zeng D., Chen Z., Yu W. Impact of left atrial diameter on all-cause mortality of patients with STEMI undergoing primary percutaneous coronary intervention. Saudi Med J 2023; 44(12): 1260–1268, https://doi.org/10.15537/smj.2023.44.12.20230235.
- Goins A.E., Rayson R., Caughey M.C., Sola M., Venkatesh K., Dai X., Yeung M., Stouffer G.A. Correlation of infarct size with invasive hemodynamics in patients with ST-elevation myocardial infarction. Catheter Cardiovasc Interv 2018; 92(5): E333–E340, https://doi.org/10.1002/ccd.27625.
- Frydland M., Møller J.E., Wiberg S., Lindholm M.G., Hansen R., Henriques J.P.S., Møller-Helgestad O.K., Bang L.E., Frikke-Schmidt R., Goetze J.P., Udesen N.L.J., Thomsen J.H., Ouweneel D.M., Obling L., Ravn H.B., Holmvang L., Jensen L.O., Kjaergaard J., Hassager C. Lactate is a prognostic factor in patients admitted with suspected ST-elevation myocardial infarction. Shock 2019; 51(3): 321–327, https://doi.org/10.1097/SHK.0000000000001191.
- Geltser B.I., Shakhgeldyan K.I., Rublev V.Yu., Domzhalov I.G., Tsivanyuk M.M., Shekunova O.I. Phenotyping of risk factors and prediction of inhospital mortality in patients with coronary artery disease after coronary artery bypass grafting based on explainable artificial intelligence methods. Russian Journal of Cardiology 2023; 28(4): 5302, https://doi.org/10.15829/1560-4071-2023-5302.
- Paolisso P., Foà A., Bergamaschi L., Angeli F., Fabrizio M., Donati F., Toniolo S., Chiti C., Rinaldi A., Stefanizzi A., Armillotta M., Sansonetti A., Magnani I., Iannopollo G., Rucci P., Casella G., Galiè N., Pizzi C. Impact of admission hyperglycemia on short and long-term prognosis in acute myocardial infarction: MINOCA versus MIOCA. Cardiovasc Diabetol 2021; 20(1): 192, https://doi.org/10.1186/s12933-021-01384-6.
- Zweck E., Thayer K.L., Helgestad O.K.L., Kanwar M., Ayouty M., Garan A.R., Hernandez-Montfort J., Mahr C., Wencker D., Sinha S.S., Vorovich E., Abraham J., O’Neill W., Li S., Hickey G.W., Josiassen J., Hassager C., Jensen L.O., Holmvang L., Schmidt H., Ravn H.B., Møller J.E., Burkhoff D., Kapur N.K. Phenotyping cardiogenic shock. J Am Heart Assoc 2021; 10(14): e020085, https://doi.org/10.1161/JAHA.120.020085.
- Shetty M.K., Kunal S., Girish M.P., Qamar A., Arora S., Hendrickson M., Mohanan P.P., Gupta P., Ramakrishnan S., Yadav R., Bansal A., Zachariah G., Batra V., Bhatt D.L., Gupta A., Gupta M. Machine learning based model for risk prediction after ST-elevation myocardial infarction: insights from the North India ST elevation myocardial infarction (NORIN-STEMI) registry. Int J Cardiol 2002; 362: 6–13, https://doi.org/10.1016/j.ijcard.2022.05.023.










