Capabilities of Human Biotissue Fluorescence Spectroscopy in the Wearable Multimodal Version
Pathological processes in biotissues are characterized by a shift in metabolic homeostasis causing biochemical changes, which can be detected by fluorescence spectroscopy methods. A wide spectrum of capabilities, simple implementation, and valuable diagnostic information obtained attract considerable interest of the medical community.
The aim of the study is to analyze the current problems of fluorescence spectroscopy of biotissues and demonstrate new capabilities of this method in a wearable multimodal version for solving various problems of practical medicine.
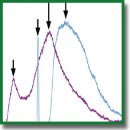
Theoretical part of the investigation. Factors influencing the registration of biotissue fluorescence have been considered. It has been established that the assessment of mitochondrial function (oxidative metabolism) by NADH and FAD fluorescence spectra is possible only under certain assumptions due to the difficulties in determining the contribution of collagen and some other fluorophores to the total spectrum. The capabilities of multimodal approach have been studied, i.e. сombining fluorescence spectroscopy and laser Doppler flowmetry in one diagnostic system as a wearable version of device implementation.
Experimental part of the investigation. To demonstrate the capabilities of the wearable analyzers of the oxidative biotissue metabolism, pilot experimental investigations have been carried out involving 8 conditionally healthy volunteers. Parameters of microcirculatory-tissue systems (oxidative metabolism) were recorded with a modified multimodal wearable analyzer capable of measuring the skin fluorescence spectra in a wide range from 320 to 900 nm. Skin fluorescence was registered in the region of forehead, dorsal carpal surface, the volar surface of the distal phalanx of the middle finger, and the plantar surface of the distal phalanx of the first toe at a 365 nm wavelength of exciting irradiation.
The conducted experiment has shown that despite the existing effect of biotissue hyperemia together with the level of melanin on the recorded fluorescence spectrum, the assessment of skin fluorescence intensity in dynamics and functional tests reflect changes in metabolic processes of biotissues and may be considered as a promising diagnostic criterion.
- Dunaev A.V. Mul’timodal’naya opticheskaya diagnostika mikrotsirkulyatorno-tkanevykh sistem organizma cheloveka [Multimodal optical diagnostics of microcirculatory tissue systems of the human body]. Staryy Oskol: TNT; 2022; 440 p.
- Rogatkin D.A. Physical foundations of laser clinical fluorescence spectroscopy in vivo. Meditsinskaya fizika 2014; 4: 78–96.
- Zherebtsov E.A., Dremin V.V., Zherebtsova A.I., Potapova E.V., Dunaev A.V. Fluorestsentnaya diagnostika mitokhondrial’noy funktsii v epitelial’nykh tkanyakh in vivo [Fluorescence diagnostics of mitochondrial function in epithelial tissues in vivo]. Orel: OGU imeni I.S. Turgeneva; 2008; 107 p.
- Richards-Kortum R., Sevick-Muraca E. Quantitative optical spectroscopy for tissue diagnosis. Annu Rev Phys Chem 1996; 47: 555–606, https://doi.org/10.1146/annurev.physchem.47.1.555.
- Alfano R., Tata D.B., Cordero J., Tomashefsky P., Longo F., Alfano M. Laser induced fluorescence spectroscopy from native cancerous and normal tissue. IEEE J Quantum Electron 1984; 20(12): 1507–1511, https://doi.org/10.1109/JQE.1984.1072322.
- Georgakoudi I., Jacobson B.C., Müller M.G., Sheets E.E., Badizadegan K., Carr-Locke D.L., Crum C.P., Boone C.W., Dasari R.R., Van Dam J., Feld M.S. NAD(P)H and collagen as in vivo quantitative fluorescent biomarkers of epithelial precancerous changes. Cancer Res 2002; 62(3): 682–687.
- Koenig K., Schneckenburger H. Laser-induced autofluorescence for medical diagnosis. J Fluoresc 1994; 4(1): 17–40, https://doi.org/10.1007/BF01876650.
- Croce A.C., Bottiroli G. Autofluorescence spectroscopy and imaging: a tool for biomedical research and diagnosis. Eur J Histochem 2014; 58(4): 2461, https://doi.org/10.4081/ejh.2014.2461.
- Mayevsky A., Chance B. Oxidation-reduction states of NADH in vivo: from animals to clinical use. Mitochondrion 2007; 7(5): 330–339, https://doi.org/10.1016/j.mito.2007.05.001.
- Mayevsky A. Mitochondrial function in vivo evaluated by NADH fluorescence. Springer; 2015; 276 p.
- Chance B., Williams G.R. Respiratory enzymes in oxidative phosphorylation. I. Kinetics of oxygen utilization. J Biol Chem 1955; 217(1): 383–393.
- Chance B., Williamson J.R., Jamieson D., Schoener B. Properties and kinetics of reduced pyridine nucleotide fluorescence of the isolated and in vivo rat heart. Biochem Zeit 1965; 341: 357–377.
- Alfano R.R., Das B.B., Cleary J., Prudente R., Celmer E.J. Light sheds light on cancer — distinguishing malignant tumors from benign tissues and tumors. Bull N Y Acad Med 1991; 67(2): 143–150.
- Alfano R., Tang G.C., Pradhan A., Lam W., Choy D., Opher E. Fluorescence spectra from cancerous and normal human breast and lung tissues. IEEE J Quantum Electron 1987; 23(10): 1806–1811, https://doi.org/10.1109/JQE.1987.1073234.
- Palmer G.M., Keely P.J., Breslin T.M., Ramanujam N. Autofluorescence spectroscopy of normal and malignant human breast cell lines. Photochem Photobiol 2003; 78(5): 462–469, https://doi.org/10.1562/0031-8655(2003)0780462:asonam2.0.co;2.
- Palmer S., Litvinova K., Dunaev A., Yubo J., McGloin D., Nabi G. Optical redox ratio and endogenous porphyrins in the detection of urinary bladder cancer: a patient biopsy analysis. J Biophotonics 2017; 10(8): 1062–1073, https://doi.org/10.1002/jbio.201600162.
- Panjehpour M., Julius C.E., Phan M.N., Vo-Dinh T., Overholt S. Laser-induced fluorescence spectroscopy for in vivo diagnosis of non-melanoma skin cancers. Lasers Surg Med 2002; 31(5): 367–373, https://doi.org/10.1002/lsm.10125.
- Croce A.C., Bottiroli G. Autofluorescence spectroscopy and imaging: a tool for biomedical research and diagnosis. Eur J Histochem 2014; 58(4): 2461, https://doi.org/10.4081/ejh.2014.2461.
- Apolikhina L.A., Denisova E.D., Bulgakova N.N., Kuzmin S.G., Vorozhtsov G.N. Fluorescence detection and photodynamic therapy of human papilloma virus associated diseases of female genital organs. In: Proceedings of the 6th International Congress of the World Association of Laser Therapy, WALT 2006. 2006; p. 59–61.
- Bulgakova N., Sokolov V., Telegina L., Vereshchagin K., Frank G., Chissov V. Study of laser-induced autofluorescence emission spectra from normal and malignant bronchial epithelium. Photonics Lasers Med 2013; 2(2): 93–99, https://doi.org/10.1515/plm-2013-0002.
- Rusakov I.G., Sokolov V.V., Bulgakova N.N., Ul’ianov R.V., Teplov A.A. Fluorescent diagnostic methods and superficial cancer of the urinary bladder: current status. Urologiia 2008; 3: 67–72.
- Dronova O.B., Tretyakov A.A., Mishchenko A.N., Bulgakova N.N. Laser induced autofluorescence of normal and metaplastic epithelium of esophagogastric transition at gastroesophageal reflux disease. Sibirskiy onkologicheskiy zhurnal 2008; 4: 11–16.
- Bulgakova N.N., Kazachkina N.I., Sokolov V.V., Smirnov V.V. Local fluorescence spectroscopy and detection of malignancies using laser excitation at various wavelengths. Laser Phys 2006; 16: 889–895, https://doi.org/10.1134/s1054660x06050227.
- Bulgakova N., Ulijanov R., Vereschagin K., Sokolov V., Teplov A., Rusakov I., Chissov V. In vivo local fluorescence spectroscopy in PDD of superficial bladder cancer. Medical Laser Application 2009; 24(4): 247–255, https://doi.org/10.1016/j.mla.2009.08.005.
- Harris K., Rohrbach D.J., Attwood K., Qiu J., Sunar U. Optical imaging of tissue obtained by transbronchial biopsies of peripheral lung lesions. J Thorac Dis 2017; 9(5): 1386–1392, https://doi.org/10.21037/jtd.2017.03.113.
- Braun F., Schalk R., Nachtmann M., Hien A., Frank R., Beuermann T., Methner F.J., Kränzlin B., Rädle M., Gretz N. A customized multispectral needle probe combined with a virtual photometric setup for in vivo detection of Lewis lung carcinoma in an animal model. Meas Sci Technol 2019; 30(10): 104001, https://doi.org/10.1088/1361-6501/ab24a1.
- Mathieu M.C., Toullec A., Benoit C., Berry R., Validire P., Beaumel P., Vincent Y., Maroun P., Vielh P., Alchab L., Farcy R., Moniz-Koum H., Fontaine-Aupart M.P., Delaloge S., Balleyguier C. Preclinical ex vivo evaluation of the diagnostic performance of a new device for in situ label-free fluorescence spectral analysis of breast masses. Eur Radiol 2018; 28(6): 2507–2515, https://doi.org/10.1007/s00330-017-5228-7.
- Spliethoff J.W., Evers D.J., Jaspers J.E., Hendriks B.H., Rottenberg S., Ruers T.J. Monitoring of tumor response to Cisplatin using optical spectroscopy. Transl Oncol 2014; 7(2): 230–239, https://doi.org/10.1016/j.tranon.2014.02.009.
- Ostrander J.H., McMahon C.M., Lem S., Millon S.R., Brown J.Q., Seewaldt V.L., Ramanujam N. Optical redox ratio differentiates breast cancer cell lines based on estrogen receptor status. Cancer Res 2010; 70(11): 4759–4766, https://doi.org/10.1158/0008-5472.CAN-09-2572.
- Sivabalan S., Vedeswari C.P., Jayachandran S., Koteeswaran D., Pravda C., Aruna P.R., Ganesan S. In vivo native fluorescence spectroscopy and nicotinamide adinine dinucleotide/flavin adenine dinucleotide reduction and oxidation states of oral submucous fibrosis for chemopreventive drug monitoring. J Biomed Opt 2010; 15(1): 017010, https://doi.org/10.1117/1.3324771.
- Palmer S., Litvinova K., Rafailov E.U., Nabi G. Detection of urinary bladder cancer cells using redox ratio and double excitation wavelengths autofluorescence. Biomed Opt Express 2015; 6(3): 977–986, https://doi.org/10.1364/BOE.6.000977.
- Fokkens B.T., Smit A.J. Skin fluorescence as a clinical tool for non-invasive assessment of advanced glycation and long-term complications of diabetes. Glycoconj J 2016; 33(4): 527–535, https://doi.org/10.1007/s10719-016-9683-1.
- Bos D.C., de Ranitz-Greven W.L., de Valk H.W. Advanced glycation end products, measured as skin autofluorescence and diabetes complications: a systematic review. Diabetes Technol Ther 2011; 13(7): 773–779, https://doi.org/10.1089/dia.2011.0034.
- Galkina E.M., Utts S.R. Fluorescent diagnostics in dermatology. Saratovskiy nauchno-meditsinskiy zhurnal 2013; 9(3): 566–572.
- Kang U.K., Papayan G.V., Berezin V.B., Petrishchev N.N., Galagudza M.M. Spectrometer for fluorescence-reflectance biomedical research. Opticheskiy zhurnal 2013; 80(1): 56–67, https://doi.org/10.1364/JOT.80.000040.
- Tuchin V. Opticheskaya biomeditsinskaya diagnostika. V 2 t. T. 2 [Optical biomedical diagnostics. In 2 vol. Vol. 2]. Moscow: FIZMATLIT; 2007; 368 p.
- Castro-e-Silva O., Sankarankutty A.K., Correa R.B., Ferreira J., Vollet Filho J.D., Kurachi C., Bagnato V.S. Autofluorescence spectroscopy in liver transplantation: preliminary results from a pilot clinical study. Transplant Proc 2008; 40(3): 722–725, https://doi.org/10.1016/j.transproceed.2008.03.005.
- Ershova E.Y., Karimova L.N., Kharnas S.S., Kuzmin S.G., Loschenov V.B. Photodynamic therapy of acne vulgaris. In: Lasers in surgery: advanced characterization, therapeutics, and systems XIII. SPIE; 2003; p. 62–67.
- De Veld D.C., Witjes M.J., Sterenborg H.J., Roodenburg J.L. The status of in vivo autofluorescence spectroscopy and imaging for oral oncology. Oral Oncol 2005; 41(2): 117–131, https://doi.org/10.1016/j.oraloncology.2004.07.007.
- Akbar N., Sokolovski S., Dunaev A., Belch J.J., Rafailov E., Khan F. In vivo noninvasive measurement of skin autofluorescence biomarkers relate to cardiovascular disease in mice. J Microsc 2014; 255(1): 42–48, https://doi.org/10.1111/jmi.12135.
- Tarakanchikova Y., Stelmashchuk O., Seryogina E., Piavchenko G., Zherebtsov E., Dunaev A., Popov A., Meglinski I. Allocation of rhodamine-loaded nanocapsules from blood circulatory system to adjacent tissues assessed in vivo by fluorescence spectroscopy. Laser Phys Lett 2018; 15: 105601, https://doi.org/10.1088/1612-202x/aad857.
- Lin Y., Gao H., Nalcioglu O., Gulsen G. Fluorescence diffuse optical tomography with functional and anatomical a priori information: feasibility study. Phys Med Biol 2007; 52(18): 5569–5585, https://doi.org/10.1088/0031-9155/52/18/007.
- Rogatkin D.A., Prisnyakova O.A., Moiseeva L.G., Cherkasov A.S. Analysis of the accuracy of clinical laser fluorescence diagnosis. Izmeritel’naya tekhnika 1998; 7: 58–61.
- Sinichkin Y.P., Utz S.R., Mavliutov A.H., Pilipenko H.A. In vivo fluorescence spectroscopy of the human skin: experiments and models. J Biomed Opt 1998; 3(2): 201–211, https://doi.org/10.1117/1.429876.
- Konig K., Riemann I. High-resolution multiphoton tomography of human skin with subcellular spatial resolution and picosecond time resolution. J Biomed Opt 2003; 8(3): 432–439, https://doi.org/10.1117/1.1577349.
- Dunaev A.V., Dremin V.V., Zherebtsov E.A., Rafailov I.E., Litvinova K.S., Palmer S.G., Stewart N.A., Sokolovski S.G., Rafailov E.U. Individual variability analysis of fluorescence parameters measured in skin with different levels of nutritive blood flow. Med Eng Phys 2015; 37(6): 574–583, https://doi.org/10.1016/j.medengphy.2015.03.011.
- Dremin V.V., Dunaev A.V. How the melanin concentration in the skin affects the fluorescence-spectroscopy signal formation. J Opt Technol 2016; 83: 43–48, https://doi.org/10.1364/JOT.83.000043.
- Parshakova V.E., Zharkikh E.V., Loktionova Yu.I., Koskin A.V., Dunaev A.V. Study of physiologic variabity of microcirculatory-tissue systems parameters of human organism using multimodal portable analyzers. Fundamental’nye i prikladnye problemy tekhniki i tekhnologii 2024; 2(364): 165–176.
- Na R., Stender I.M., Ma L., Wulf H.C. Autofluorescence spectrum of skin: component bands and body site variations. Skin Res Technol 2000; 6(3): 112–117, https://doi.org/10.1034/j.1600-0846.2000.006003112.x.
- Kollias N., Zonios G., Stamatas G.N. Fluorescence spectroscopy of skin. Vib Spectrosc 2002; 28(1): 17–23, https://doi.org/10.1016/S0924-2031(01)00142-4.
- Ryzhkova E., Morgunova T., Potapova E., Ryzhkov I., Fadeyev V. Fluorescence spectroscopy with temperature functional tests in the assessment of markers of intracellular energy metabolism: spatial heterogeneity and reproducibility of measurements. J Biophotonics 2024; 17(10): e202400294, https://doi.org/10.1002/jbio.202400294.
- Gillies R., Zonios G., Anderson R.R., Kollias N. Fluorescence excitation spectroscopy provides information about human skin in vivo. J Invest Dermatol 2000; 115(4): 704–707, https://doi.org/10.1046/j.1523-1747.2000.00091.x.
- Potapova E.V., Dremin V.V., Zherebtsov E.A., Makovik I.N., Zharkikh E.V., Dunaev A.V., Pilipenko O.V., Sidorov V.V., Krupatkin A.I. A complex approach to noninvasive estimation of microcirculatory tissue impairments in feet of patients with diabetes mellitus using spectroscopy. Optics and Spectroscopy 2017; 123(6): 955–964, https://doi.org/10.1134/s0030400x1712013x.
- Dremin V.V. Analytical review of approaches to mathematical modeling of biological tissue fluorescence. Fundamental’nye i prikladnye problemy tekhniki i tekhnologii 2016; 6(320): 92–102.
- Dremin V.V., Zherebtsov E.A., Sidorov V.V., Krupatkin A.I., Makovik I.N., Zherebtsova A.I., Zharkikh E.V., Potapova E.V., Dunaev A.V., Doronin A.A., Bykov A.V., Rafailov I.E., Litvinova K.S., Sokolovski S.G., Rafailov E.U. Multimodal optical measurement for study of lower limb tissue viability in patients with diabetes mellitus. J Biomed Opt 2017; 22(8): 1–10, https://doi.org/10.1117/1.JBO.22.8.085003.
- Dunajev A.V., Drjomin V.V., Gherebtsov E.A., Palmer S.G., Sokolowskiy S.G., Rafailov E.U. Analisys of individual variability of parameters of laser fluorescence diagnostics. Biotekhnosfera 2013; 2(26): 38–45.
- Dunaev A. Wearable devices for multimodal optical diagnostics of microcirculatory-tissue systems: application experience in the clinic and space. J Biomed Photonics Eng 2023; 9(2): 020201, https://doi.org/10.18287/JBPE23.09.020201.
- Sidorov V.V., Rybakov Y.L., Gukasov V.M., Evtushenko G.S. A system of local analyzers for noninvasive diagnostics of the general state of the tissue microcirculation system of human skin. Biomed Eng (NY) 2022; 55(6): 379–382.
- Dunaev A.V. Principles of construction of technical means multiparametric optical diagnostics for assessing the functional state of microcirculatory-tissue systems. Fundamental’nye i prikladnye problemy tekhniki i tekhnologii 2020; 344(6): 131–140.
- Loktionova Yu.I., Zharkikh E.V., Zherebtsova A.I., Kozlov I.O., Zherebtsov E.A., Masalygina G.I., Dunaev A.V. Study of age-related and pathological features of microhemodynamics in healthy volunteers and patients with type 2 diabetes mellitus by wearable laser Doppler flowmetry devices. Fundamental’nye i prikladnye problemy tekhniki i tekhnologii 2019; 120: 13–20.
- Gorshkov A.Yu., Korolev A.I., Fedorovich A.A., Omelyanenko K.V., Dadaeva V.A., Drapkina O.M. Parameters of skin perfusion according to the data of remote laser doppler flowmetry in men with newly detected arterial hypertension. Profilakticheskaya meditsina 2022; 25(5–2): 19–20.
- Fedorovich A.A., Markov D.S., Malishevsky M.V., Yudakov O.O., Gorshkov A.Yu., Baldin A.V., Zhuk D.M., Spasenov A.Yu., Korolev A.I., Koptelov A.V., Drapkina O.M. Microcirculatory disorders in the forearm skin in the acute phase of COVID-19 according to laser Doppler flowmetry. Regional blood circulation and microcirculation 2022; 21(3): 56–63, https://doi.org/10.24884/1682-6655-2022-21-3-56-63.
- Saha M., Dremin V., Rafailov I., Dunaev A., Sokolovski S., Rafailov E. Wearable laser doppler flowmetry sensor: a feasibility study with smoker and non-smoker volunteers. Biosensors (Basel) 2020; 10(12): 201, https://doi.org/10.3390/bios10120201.
- Zharkikh E.V., Loktionova Yu.I., Sidorov V.V., Krupatkin A.I., Masalygina G.I., Dunaev A.V. Control of blood microcirculation parameters in therapy with alpha-lipoic acid in patients with diabetes mellitus. Human Physiology 2022; 48(4): 456–464, https://doi.org/10.1134/s0362119722040156.
- Frolov A.V., Loktionova Yu.I., Zharkikh E.V., Sidorov V.V., Krupatkin A.I., Dunaev A.V. Investigation of changes in the skin blood microcirculation when performing the hatha yoga breathing technique. Regional blood circulation and microcirculation 2021; 20(4): 33–44, https://doi.org/10.24884/1682-6655-2021-20-4-33-44.










