Poly-D,L-Lactide-co-Glycolide and Sodium Enoxaparin Composition — an Advanced Coating for Vascular Stents: Biocompatibility and Efficiency Assessment of Stent-Grafts in an Experiment on Large Animals
The aim of the study was to evaluate the biocompatibility of vascular stents coated with the membrane based on a copolymer of poly-D,L-lactide-co-glycolide and sodium enoxaparin in an experiment on large animals.
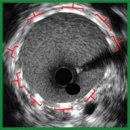
Materials and Methods. A biodegradable coating based on a copolymer of poly-D,L-lactide-co-glycolide (the polylactide-glycolide ratio — 50:50) and low-molecular sodium enoxaparin was applied on 8-mm-long metallic coronary Calipso stents by electrospinning. The sheep carotid artery was implanted with the coated stents (stent-grafts) and uncoated stents. The dynamic patency was assessed by color duplex ultrasound. Three months later, the artery–stent fragments were explanted, fixed with buffered formalin with post-fixation with osmium tetroxide, dehydrated in ethanol and acetone followed by impregnating with epoxy resin. After polymerization, the samples were ground and polished to the required depth. To enhance the contrast after polishing, the samples were treated with Reynolds lead citrate. The samples were visualized by scanning electron microscopy in the backscattered electron mode.
Results. During the three-month experiment, no cases of thrombosis or stenosis of stents and stent-grafts were revealed. A uniform dense neointima up to 165 μm thick formed on the internal surface of the stent-grafts, it was twice as thick as the intima of the intact carotid artery adjacent to the stent-graft. A loose neointima formed on the inner part of the stents without a polymer membrane, reaching 380 μm in some places. All samples demonstrated a classic picture of the formation of a dense fibrous capsule, which separated the metal stent struts from the blood flow and structural elements of the artery, however, the morphology and cellular composition in the samples varied significantly. The struts of the stents without a membrane were surrounded by numerous inflammatory cells. The environment of the stent grafts was represented mainly by smooth muscle cells, fibrocytes, fragments of the elastic membrane located in the intercellular matrix; there were no inflammatory cells. The polymer coating of the stent-grafts completely degraded forming no scar tissue.
Conclusion. The developed polymer coating based on a copolymer of poly-D,L-lactide-co-glycolide (the polylactide-glycolide ratio — 50:50) and the low-molecular sodium enoxaparin for a vascular stent appeared to be effective. When implanted in sheep carotid arteries, the stent-grafts cause no development of thrombosis and stenosis, successfully integrating with the animal artery. In 3 months, complete resorption of the polymer coating occurred with no signs of a chronic inflammatory reaction.
- Timmis A., Townsend N., Gale C.P., Torbica A., Lettino M., Petersen S.E., Mossialos E.A., Maggioni A.P., Kazakiewicz D., May H.T., De Smedt D., Flather M., Zuhlke L., Beltrame J.F., Huculeci R., Tavazzi L., Hindricks G., Bax J., Casadei B., Achenbach S., Wright L., Vardas P.; European Society of Cardiology. European Society of Cardiology: cardiovascular disease statistics 2019. Eur Heart J 2020; 41(1): 12–85, https://doi.org/10.1093/eurheartj/ehz859.
- Alekyan B.G., Boytsov S.A., Manoshkina E.M., Ganyukov V.I. Myocardial revascularization in Russian Federation for acute coronary syndrome in 2016–2020. Kardiologiia 2021; 61(12): 4–15, https://doi.org/10.18087/cardio.2021.12.n1879.
- Collet J.P., Thiele H., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., Gale C.P., Gilard M., Jobs A., Jüni P., Lambrinou E., Lewis B.S., Mehilli J., Meliga E., Merkely B., Mueller C., Roffi M., Rutten F.H., Sibbing D., Siontis G.C.M.; ESC Scientific Document Group 2020. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021; 42(14): 1289–1367, https://doi.org/10.1093/eurheartj/ehaa575.
- Ryabov V.V., Kretov E.I., Popov S.V., Khassanov I.Sh., Yakovlev M.Yu. Coronary stent technology and the role of inflammation in the atherogenesis: problems and prospects. Bulletin of Siberian Medicine 2021; 20(1): 200–212, https://doi.org/10.20538/1682-0363-2021-1-200-212.
- Lemmert M.E., van Bommel R.J., Diletti R., Wilschut J.M., de Jaegere P.P., Zijlstra F., Daemen J., Van Mieghem N.M. Clinical characteristics and management of coronary artery perforations: a single-center 11-year experience and practical overview. J Am Heart Assoc 2017; 6(9): e007049, https://doi.org/10.1161/JAHA.117.007049.
- Rao G., Sheth S., Grines C. Percutaneous coronary intervention: 2017 in review. J Interv Cardiol 2018; 31(2): 117–128, https://doi.org/10.1111/joic.12508.
- Patel V.G., Brayton K.M., Tamayo A., Mogabgab O., Michael T.T., Lo N., Alomar M., Shorrock D., Cipher D., Abdullah S., Banerjee S., Brilakis E.S. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv 2013; 6(2): 128–136, https://doi.org/10.1016/j.jcin.2012.10.011.
- Kufner S., Schacher N., Ferenc M., Schlundt C., Hoppmann P., Abdel-Wahab M., Mayer K., Fusaro M., Byrne R.A., Kastrati A. Outcome after new generation single-layer polytetrafluoroethylene-covered stent implantation for the treatment of coronary artery perforation. Catheter Cardiovasc Interv 2019; 93(5): 912–920, https://doi.org/10.1002/ccd.27979.
- Chen S., Lotan C., Jaffe R., Rubinshtein R., Ben-Assa E., Roguin A., Varshitzsky B., Danenberg H.D. Pericardial covered stent for coronary perforations. Catheter Cardiovasc Interv 2015; 86(3): 400–404, https://doi.org/10.1002/ccd.26011.
- Kandzari D.E., Birkemeyer R. PK Papyrus covered stent: device description and early experience for the treatment of coronary artery perforations. Catheter Cardiovasc Interv 2019; 94(4): 564–568, https://doi.org/10.1002/ccd.28306.
- Agathos E.A., Tomos P.I., Kostomitsopoulos N., Koutsoukos P.G. Calcitonin as an anticalcification treatment for implantable biological tissues. J Cardiol 2019; 73(2): 179–182, https://doi.org/10.1016/j.jjcc.2018.07.010.
- Glushkova T.V., Ovcharenko E.A., Sevostyanova V.V., Klyshnikov K.Yu. Features of calcification of valves heart and their biological prostheses: composition, structure and localization of calcifications. Kardiologiia 2018; 58(5): 72–81, https://doi.org/10.18087/cardio.2018.5.10110.
- Rezvova M.A., Ovcharenko E.A., Klyshnikov K.Y., Glushkova T.V., Kostyunin A.E., Shishkova D.K., Matveeva V.G., Velikanova E.A., Shabaev A.R., Kudryavtseva Y.A. Electrospun bioresorbable polymer membranes for coronary artery stents. Front Bioeng Biotechnol 2024; 12: 1440181, https://doi.org/10.3389/fbioe.2024.1440181.
- Shabaev A.R., Kanonykina A.Yu., Bogdanov L.A., Shishkova D.K., Kudryavtseva Yu.A. Selection of polymer for stent-graft coating in terms of biocompatibility and biodegradation characteristics. Complex Issues of Cardiovascular Diseases 2024; 13(4): 77–89, https://doi.org/10.17802/2306-1278-2024-13-4-77-89.
- Hao K., Sang L., Ding L., Shen X., Fu D., Qi X. Enoxaparin sodium bone cement displays local anti-inflammatory effects by regulating the expression of IL-6 and TNF-α. Heliyon 2023; 9(6): e16530, https://doi.org/10.1016/j.heliyon.2023.e16530.
- Nakamura K., Keating J.H., Edelman E.R. Pathology of endovascular stents. Interv Cardiol Clin 2016; 5(3): 391–403, https://doi.org/10.1016/j.iccl.2016.02.006.
- Mukhamadiyarov R.A., Evtushenko A.V., Tarasov R.S., Khalivopulo I.K., Lyapin A.A., Kutikhin A.G. Structure of neointima in bare metal stents and expanded poly (tetrafluoroethylene) patches in children after two-step surgical treatment of tetralogy of Fallot. Clinical and Experimental Surgery. Petrovsky Journal 2022; 10(3): 64–75, https://doi.org/10.33029/2308-1198-2022-10-3-64-75.
- Shurygina I.A., Shurygin M.G., Ayushinova N.I., Kanya O.V. Fibroblasts and their role in the development of connective tissue. Sibirskiy meditsinskiy zhurnal (Irkutsk) 2012, 3: 8–12.
- Sorokoumova M.V., Kompantsev D.V., Shcherbakova L.I., Kompantsev V.A., Medvetsky A.I., Zyablitseva N.S., Vasina T.M., Sannikova E.G. Poly-D,L-lactide-co-glycolide — a prospective polymer for the development of nanosystems for drug delivery (review). Medical & Pharmaceutical Journal “Pulse” 2022; 24(8): 42–52, https://doi.org/10.26787/nydha-2686-6838-2022-24-8-42-52.










