The Advantages of Continuous Epidural Anesthesia in Spinal Deformity Surgery
The aim of the investigation was to assess the efficacy of epidural anesthesia and analgesia during the integrated anesthetic management in spinal deformity surgery.
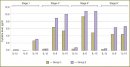
Materials and Methods. The prospective randomized study involved 350 patients aged from 15 to 65 years, divided into two groups: group 1 (n=205) were given combined anesthesia — epidural and endotracheal anesthesia with sevoflurane and continuous epidural analgesia with ropivacaine, fentanyl and epinephrine after surgery; group 2 (n=145) had general anesthesia with sevoflurane and fentanyl, and systemic administration of opioids after surgery. We assessed systemic hemodynamics parameters (a non-invasive method), pain at rest and activities, parameters of hemostasis and fibrinolysis, plasma levels of stress hormones, cytokine levels at seven stages of the study (before, during and three days after surgery).
Results. Patients in group 1 with epidural anesthesia had significantly less pain both at rest and motion. The most blood saving effect (up to 60% of blood loss) was also found in group 1. Hemodynamic monitoring demonstrated epidural anesthesia not to lead to the life-threatening events of myocardial contractility, cardiac output, systemic vascular resistance and critical increasing of extravascular lung water. The impact of epidural anesthesia on hemostasis encompassed the activation of both coagulation and fibrinolysis. Furthermore, patients in group 1 compared to group 2 had significantly lower plasma levels of glucose, lactate, С-reactive protein, cortisol, and interleukins IL-1β, IL-6, IL-10.
Conclusion. Comprehensive anesthetic protection in spinal deformity surgery based on epidural anesthesia provides adequate antinociceptive effects, inhibition of endocrine and metabolic stress response and correction of hemostasis problems.
- Mikhaylovskiy M.V., Lebedeva M.N., Sadovaya T.N., et al. Short- and long-term results of surgical treatment of patients with severe idiopathic scoliosis. Khirurgiya pozvonochnika 2009; 2: 38–47.
- Bird S., McGill N. Blood conservation and pain control in scoliosis corrective surgery: an online survey of UK practice. Paediatr Anaesth 2011 Jan; 21(1): 50–53, http://dx.doi.org/10.1111/j.1460-9592.2010.03443.x.
- Lebedeva M.N. Massive blood loss as a risk factor in scoliosis surgery: the ways of problem solution. Khirurgiya pozvonochnika 2009; 4: 70–79.
- Ahlers O., Nachtigall I., Lenze J., et al. Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br J Anaesth 2008 Dec; 101(6): 781–787, http://dx.doi.org/10.1093/bja/aen287.
- Kawasaki T., Ogata M., Kawasaki C., et al. Effects of epidural anaesthesia on surgical stress-induced immunosuppression during upper abdominal surgery. Br J Anaesth 2007; 98(2): 196–203, http://dx.doi.org/10.1093/bja/ael334.
- Yokoyama M., Itano Y., Katayama H., et al. The effects of continuous epidural anesthesia and analgesia on stress response and immune function in patients undergoing radical esophagectomy. Anesth Analg 2005; 101(5): 1521–1527, http://dx.doi.org/10.1213/01.ANE.0000184287.15086.1E.
- Volk T., Döpfmer U.R., Schmutzler M., et al. Stress induced IL-10 does not seem to be essential for early monocyte deactivation following cardiac surgery. Cytokine 2003; 24(6): 237–243, http://dx.doi.org/10.1016/S1043-4666(03)00090-5.
- Volk T., Schenk M., Voigt K., et al. Postoperative epidural anesthesia preserves lymphocyte, but not monocyte, immune function after major spine surgery. Anesth Analg 2004; 98: 1086–1092, http://dx.doi.org/10.1213/01.ANE.0000104586.12700.3A.
- Qu D.M., Jin Y.F., Ye T.H., et al. The effects of general anesthesia combined with epidural anesthesia on the stress response in thoracic surgery. Zhonghua Yi Xue Za Zhi 2003; 83(5): 408–411.
- Lyuboshevskiy P.A., Artamonova N.I., Zabusov A.V., Denisenko I.L. Hemostatic disorders in major abdominal surgery: the role of regional anesthesia. Regionarnaya anesteziya i lechenie ostroy boli 2009; 2(3): 20–26.
- Hahnenkamp K., Theilmeier G., Van Aken H.K., Hoenemann C.W. The effects of local anesthetics on perioperative coagulation, inflammation, and microcirculation. Anesth Analg 2002; 94(6): 1441–1447, http://dx.doi.org/10.1213/00000539-200206000-00011.
- Ulke Z.S., Sentrk M. Non-analgesic effects of thoracic epidural anesthesia. Agri 2007 Apr; 19(2): 6–12.
- Wang T.L., Qi Y.Q., Yang B.X., Zhao L. Epidural anesthesia can protect fibrinolytic function after surgery. Beijing Da Xue Xue Bao 2004; 36(4): 383–389.
- Choi S., Rampersaud Y.R., Chan V.W., et al. The addition of epidural local anesthetic to systemic multimodal analgesia following lumbar spinal fusion: a randomized controlled trial. Can J Anaesth 2014 Apr; 61(4): 330–339, http://dx.doi.org/10.1007/s12630-014-0115-z.
- Sundarathiti P., Pasutharnchat K., Jommaroeng P. Thoracic epidural-general analgesia in scoliosis surgery. J Clin Anesth 2010 Sep; 22(6): 410–414.
- Lee Y.C., Park S.J., Kim J.S., Cho C.H. Effect of tranexamic acid on reducing postoperative blood loss in combined hypotensive epidural anesthesia and general anesthesia for total hip replacement. J Clin Anesth 2013 Aug; 25(5): 393–398, http://dx.doi.org/10.1016/j.jclinane.2013.02.006.
- März P., Ozbek S., Fischer M., et al. Differential response of neuronal cells to a fusion protein of ciliary neurotrophic factor/soluble CNTF-receptor and leukemia inhibitory factor. Eur J Biochem 2002 Jun; 269(12): 3023–3031, http://dx.doi.org/10.1046/j.1432-1033.2002.02977.x.
- Kao L.S., Phatak U.R. Glycemic control and prevention of surgical site infection. Surg Infect (Larchmt) 2013 Oct; 14(5): 437–444, http://dx.doi.org/10.1089/sur.2013.008.
- Wang T.L., Qi Y.Q., Yang B.X., Zhao L. Epidural anesthesia can protect fibrinolytic function after surgery. Beijing Da Xue Xue Bao 2004 Aug 18; 36(4): 383–389.
- Raw D.A., Beattie J.K., Hunter J.M. Anaesthesia for spinal surgery in adults. Br J Anaesth 2003; 91(6): 886–904, http://dx.doi.org/10.1093/bja/aeg253.










