Bisphosphonates as Potential Inhibitors of Calcification in Bioprosthetic Heart Valves (Review)
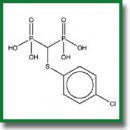
As early as 50 years ago, bisphosphonates turned from a water treatment agent into one of the most widely used groups of drugs for the treatment of various diseases of calcium metabolism (bone tissue resorption, oncological complications of neurodegenerative diseases and others). Years of research on bisphosphonates have contributed to the understanding of their molecular and cellular pathways of their action. All bisphosphonates have a similar structure and common properties, however, there are obvious chemical, biochemical, and pharmacological differences between them. Each bisphosphonate has its own unique profile. This review summarizes data on the mechanisms of action of bisphosphonates, demonstrates the experience and prospects for their use for the modification of cardiovascular bioprostheses, since the issue of preventing bisphosphonate calcification has not been settled yet.
- McClung М. Bisphosphonates. Arq Bras Endocrinol Metab 2006; 50(4): 735–744, https://doi.org/10.1590/s0004-27302006000400018.
- Bishop N.J., Russell R.G.G. Bisphosphonates. In: Osteogenesis imperfecta. Shapiro J.R., Byers P.H., Glorieux F.H., Sponseller P.D. (editors). Cambridge, Massachusetts: Academic Press; 2014; p. 495–500, https://doi.org/10.1016/b978-0-12-397165-4.00053-8.
- Peris P., Monegal A., Guañabens N. Bisphosphonates in inflammatory rheumatic diseases. Bone 2021; 146: 11588, https://doi.org/10.1016/j.bone.2021.115887.
- Shi M., Chen L., Wu H., Wang Y., Wang W., Zhang Y., Yan S. Effect of bisphosphonates on periprosthetic bone loss after total knee arthroplasty: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 2018; 19(1): 177, https://doi.org/10.1186/s12891-018-2101-z.
- Zameer S., Najmi A.K., Vohora D., Akhtar M. Bisphosphonates: future perspective for neurological disorders. Pharmacol Rep 2018; 70(5): 900–907, https://doi.org/10.1016/j.pharep.2018.03.011.
- Biggin A., Munns C.F. Long-term bisphosphonates therapy in osteogenesis imperfecta. Curr Osteoporos Rep 2017; 15(5): 412–418, https://doi.org/10.1007/s11914-017-0401-0.
- Zhabina A.S. The role of bisphosphonates in the prevention and treatment of bone metastases. Prakticeskaa onkologia 2011; 12(3): 124–131.
- Coleman R. Bisphosphonates and breast cancer — from cautious palliation to saving lives. Bone 2020; 140: 115570, https://doi.org/10.1016/j.bone.2020.115570.
- Chapurlat R., Legrand M.A. Bisphosphonates for the treatment of fibrous dysplasia of bone. Bone 2021; 143: 115784, https://doi.org/10.1016/j.bone.2020.115784.
- Ralston S.H. Bisphosphonates in management of Paget’s disease. Bone 2020; 138: 115465, https://doi.org/10.1016/j.bone.2020.115465.
- Sedghizadeh P.P., Sun S., Jones A.C., Sodagar E., Cherian P., Chen C., Junka A.F., Neighbors J.D., McKenna C.E., Russell R.G.G., Ebetino F.H. Bisphosphonates in dentistry: historical perspectives, adverse effects, and novel applications. Bone 2021; 147: 115933, https://doi.org/10.1016/j.bone.2021.115933.
- Suva L.J., Cooper A., Watts A.E., Ebetino F.H., Price J., Gaddy D. Bisphosphonates in veterinary medicine: the new horizon for use. Bone 2021; 142: 115711, https://doi.org/10.1016/j.bone.2020.115711.
- Ossipov D.A. Bisphosphonate-modified biomaterials for drug delivery and bone tissue engineering. Expert Opin Drug Deliv 2015; 12(9): 1443–1458, https://doi.org/10.1517/17425247.2015.1021679.
- Compston J. Practical guidance for the use of bisphosphonates in osteoporosis. Bone 2020; 136: 115330, https://doi.org/10.1016/j.bone.2020.115330.
- Brufsky A., Marti J.L.G., Nasrazadani A., Lotze M.T. Boning up: amino-bisphophonates as immunostimulants and endosomal disruptors of dendritic cell in SARS-CoV-2 infection. J Transl Med 2020; 18(1): 261, https://doi.org/10.1186/s12967-020-02433-6.
- Russell R.G.G. Bisphosphonates: the first 40 years. Bone 2011; 49(1): 2–19, https://doi.org/10.1016/j.bone.2011.04.022.
- Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev 1998; 9(1): 80–100, https://doi.org/10.1210/edrv.19.1.0325.
- Li Q., Kingman J., Sundberg J.P., Levine M.A., Uitto J. Dual effects of bisphosphonates on ectopic skin and vascular soft tissue mineralization versus bone microarchitecture in a mouse model of generalized arterial calcification of infancy. J Invest Dermatol 2016; 136(1): 275–283, https://doi.org/10.1038/jid.2015.377.
- Orriss I.R., Arnett T.R., Russell R.G.G. Pyrophosphate: a key inhibitor of mineralization. Curr Opin Pharmacol 2016; 28: 57–68, https://doi.org/10.1016/j.coph.2016.03.003.
- Green J.R. Bisphosphonates: preclinical review. Oncologist 2004; 9(S4): 3–13, https://doi.org/10.1634/theoncologist.9-90004-3.
- Papapoulos S.E. Bisphosphonates: how do they work? Best Pract Res Clin Endocrinol Metab 2008; 22(5): 831–847, https://doi.org/10.1016/j.beem.2008.07.001.
- Cremers S., Papapoulos S. Pharmacology of bisphosphonates. Bone 2011; 49(1): 42–49, https://doi.org/10.1016/j.bone.2011.01.014.
- Ebetino F.H., Hogan A.M.L., Sun S., Tsoumpra M.K., Duan X., Triffitt J.T., Kwaasi A.A., Dunford J.E., Barnett B.L., Oppermann U., Lundy M.W., Boyde A., Kashemirov B.A., McKenna C.E., Russell R.G.G. The relationship between the chemistry and biological activity of the bisphosphonates. Bone 2011; 49(1): 20–33, https://doi.org/10.1016/j.bone.2011.03.774.
- Eriksen E.F., Halse J. When should bisphosphonate treatment be discontinued? Tidsskr Nor Laegeforen 2012; 132(14): 1630–1632, https://doi.org/10.4045/tidsskr.11.0788.
- Puljula E., Turhanen P., Vepsäläinen J., Monteil M., Lecouvey M., Weisell J. Structural requirements for bisphosphonate binding on hydroxyapatite: NMR study of bisphosphonate partial esters. ACS Med Chem Lett 2015; 6(4): 397–401, https://doi.org/10.1021/ml5004603.
- Henneman Z.J., Nancollas G.H., Ebetino F.H., Russell R.G.G., Phipps R.J. Bisphosphonate binding affinity as assessed by inhibition of carbonated apatite dissolution in vitro. J Biomed Mater Res A 2008; 85(4): 993–1000, https://doi.org/10.1002/jbm.a.31599.
- Lawson M.A., Xia Z., Barnett B.L., Triffitt J.T., Phipps R.J., Dunford J.E., Locklin R.M., Ebetino F.H., Russell R.G.G. Differences between bisphosphonates in binding affinities for hydroxyapatite. J Biomed Mater Res B Appl Biomater 2010; 92(1): 149–155, https://doi.org/10.1002/jbm.b.31500.
- Kuźnik A., Październiok-Holewa A., Jewula P., Kuźnik N. Bisphosphonates — much more than only drugs for bone diseases. Eur J Pharmacol 2010; 866: 172773, https://doi.org/10.1016/j.ejphar.2019.172773.
- Alwahhabi B.K., Alsuwaine B.A. Long-term use of bisphosphonates in osteoporosis. Saudi Med J 2017; 38(6): 604–608, https://doi.org/10.15537/smj.2017.6.19793.
- Cremers S., Pillai G., Papapoulos S.E. Pharmacokinetics/pharmacodynamics of bisphosphonates. Clin Pharmacokinet 2005; 44(6): 551–570, https://doi.org/10.2165/00003088-200544060-00001.
- Cremers S., Drake M.T., Ebetino F.H., Bilezikian J.P., Russell R.G.G. Pharmacology of bisphosphonates. Br J Clin Pharmacol 2019; 85(6): 1052–1062, https://doi.org/10.1111/bcp.13867.
- Baron R., Ferrari S., Russell R.G.G. Denosumab and bisphosphonates: different mechanisms of action and effects. Bone 2011; 48(4): 677–692, https://doi.org/10.1016/j.bone.2010.11.020.
- Cremers S., Ebetino F.H., Phipps R. On the pharmacological evaluation of bisphosphonates on humans. Bone 2020; 139: 11550, https://doi.org/10.1016/j.bone.2020.115501.
- Russell R.G.G., Watts N.B., Ebetino F.H., Rogers M.J. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 2008; 19(6): 733–759, https://doi.org/10.1007/s00198-007-0540-8.
- Watts N.B., Chessnut C.H. III, Genant H.K., Harris S.T., Jackson R.D., Licata A.A., Miller P.D., Mysiw W.J., Richmond B., Valent D. History of etidronate. Bone 2020; 134: 115222, https://doi.org/10.1016/j.bone.2020.115222.
- Dunford J.E., Kavanagh K., Oppermann U., Ebetino F.H., Russell R.G.G., Rogers M.J. Investigations into the kinetic mechanism of inhibition of farnesyl diphosphate synthase by nitrogen containing bisphosphonates. Bone 2006; 38(3 Suppl 1): 47–48, https://doi.org/10.1016/j.bone.2005.12.037.
- Clarke B.L. The molecular mechanism of nitrogen-containing bisphosphonates as antiosteoporosis drugs. Yearbook of Endocrinology 2007; 2007: 330–331, https://doi.org/10.1016/s0084-3741(08)70151-3.
- Papapoulos S.E. Pamidronate: a model compound of the pharmacology of nitrogen-containing bisphosphonates; a Leiden historical perspective. Bone 2020; 134: 115244, https://doi.org/10.1016/j.bone.2020.115244.
- Dunford J.E., Kwaasi A.A., Rogers M.J., Barnett B.L., Ebetino F.H., Russell R.G.G., Oppermann U., Kavanagh K.L. Structure–activity relationships among the nitrogen containing bisphosphonates in clinical use and other analogues: time-dependent inhibition of human farnesyl pyrophosphate synthase. J Med Chem 2008; 51(7): 2187–2195, https://doi.org/10.1021/jm7015733.
- Knyaz’kova I.I. Clinical pharmacology of bisphosphonates. Farmakoterapіya 2014; 5(6): 181–182.
- Baroncelli G.I., Bertelloni S. The use of bisphosphonates in pediatrics. Horm Res Paediatr 2014; 82(5): 290–302, https://doi.org/10.1159/000365889.
- Pazianas M., van der Geest S., Miller P. Bisphosphonates and bone quality. BoneKEy Rep 2014; 3, https://doi.org/10.1038/bonekey.2014.24.
- McCloskey E., Paterson A.H., Powles T., Kanis J.A. Clodronate. Bone 2021; 143: 115715, https://doi.org/10.1016/j.bone.2020.115715.
- Cummings S.R., Santora A.C., Black D.M., Russell R.G.G. History of alendronate. Bone 2020; 137: 115411, https://doi.org/10.1016/j.bone.2020.115411.
- Fleurence R.L., Iglesias C.L., Johnson J.M. The cost effectiveness of bisphosphonates for the prevention and treatment of osteoporosis. Pharmacoeconomics 2007; 25(11): 913–933, https://doi.org/10.2165/00019053-200725110-00003.
- Fuggle N.R., Curtis B., Clynes M., Zhang J., Ward K., Javaid M.K., Harvey N.C., Dennison E., Cooper C. The treatment gap: the missed opportunities for osteoporosis therapy. Bone 2021; 144: 115833, https://doi.org/10.1016/l.bone.2020.115833.
- Purohit O.P., Radstone C.R., Anthony C., Kanis J.A., Coleman R.E. A randomised double-blind comparison of intravenous pamidronate and clodronate in the hypercalcaemia of malignancy. Br J Cancer 1995; 72(5): 1289–1293, https://doi.org/10.1038/bjc.1995.502.
- McClung M., Omizo M., Minkoff J., Fiske D., Kriegman A., Beamer E., Zhou W. Single infusion of zoledronic acid 5 mg provides sustained benefits in bone mineral density and biomarkers at 12 months in postmenopausal women with low bone mineral density and prior alendronate therapy. J Clin Densitom 2007; 10(2): S220–S221, https://doi.org/10.1016/j.jocd.2007.03.082.
- Dhillon S., Lyseng-Williamson K.A. Zoledronic acid.Drugs 2008; 68(4): 507–534, https://doi.org/10.2165/00003495-200868040-00010.
- Djordjevic D. Benefits of use of zoledronic acid in carcinoma prostate bone metastases (zoledronic acid). Serb J Anesth Intensive Ther 2017; 39(7–8): 211–217, https://doi.org/10.5937/sjait1708211d.
- Anastasilakis A.D., Polyzos S.A., Efstathiadou Z.A., Savvidis M., Sakellariou G.T., Papatheodorou A., Kokkoris P., Makras P. Denosumab in treatment-naïve and pre-treated with zoledronic acid postmenopausal women with low bone mass: effect on bone mineral density and bone turnover markers. Metabolism 2015; 64(10): 1291–1297, https://doi.org/10.1016/j.metabol.2015.06.018.
- Brown J.P. Antiresorptives: safety concerns — clinical perspective. Toxicol Pathol 2017; 45(7): 859–863, https://doi.org/10.1177/0192623317737066.
- Fernández-Martín S., López-Peña M., Muñoz F., Permuy M., González-Cantalapiedra A. Bisphosphonates as disease-modifying drugs in osteoarthritis preclinical studies: a systematic review from 2000 to 2020. Arthritis Res Ther 2021; 23(1): 60, https://doi.org/10.1186/s13075-021-02446-6.
- Nancollas G.H., Tang R., Phipps R.J., Henneman Z., Gulde S., Wu W., Mangood A., Russell R.G.G., Ebetino F.H. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone 2006; 38(5): 617–627, https://doi.org/10.1016/j.bone.2005.05.003.
- Price P.A., Faus S.A., Williamson M.K. Bisphosphonates alendronate and ibandronate inhibit artery calcification at doses comparable to those that inhibit bone resorption. Arterioscler Thromb Vasc Biol 2001; 21(5): 817–824, https://doi.org/10.1161/01.atv.21.5.817.
- Price P.A., Omid N., Than T.N., Williamson M.K. The amino bisphosphonate ibandronate prevents calciphylaxis in the rat at doses that inhibit bone resorption. Calcif Tissue Int 2002; 71(4): 356–363, https://doi.org/10.1007/s00223-002-1006-9.
- Lang M., Zhou Z., Shi L., Niu J., Xu S., Lin W., Chen Z., Wang Y. Influence of zoledronic acid on proliferation, migration, and apoptosis of vascular endothelial cells. Br J Oral Maxillofac Surg 2016; 54(8): 889–893, https://doi.org/10.1016/j.bjoms.2016.05.030.
- Jensen P.R., Andersen T.L., Chavassieux P., Roux J.P., Delaisse J.M. Bisphosphonates impair the onset of bone formation at remodeling sites. Bone 2021; 145: 115850, https://doi.org/10.1016/j.bone.2021.115850.
- Bauer C., le Saux O., Pomozi V., Aherrahrou R., Kriesen R., Stölting S., Liebers A., Kessler T., Schunkert H., Erdmann J., Aherrahrou Z. Etidronate prevents dystrophic cardiac calcification by inhibiting macrophage aggregation. Sci Rep 2018; 8(1): 5812, https://doi.org/10.1038/s41598-018-24228-y.
- Russel R.G.G., Xia Z., Dunford J.E., Opperman U., Kwaasi A., Hulley P.A., Kavanagh K.L., Triffitt J.T., Lundy M.W., Phipps R.J., Barnett B.L., Coxon F.P., Rogers M.J., Watts N.B., Ebetino F.H. Bisphosphonates: an update on mechanisms of action and how these relate to clinical efficacy. Ann N Y Acad Sci 2007; 1117(1): 209–257, https://doi.org/10.1196/annals.1402.089.
- Frith J.C., Mӧnkkӧnen J., Auriola S., Mӧnkkӧnen H., Rogers M.J. The molecular mechanism of action of the antiresorptive and antiinflammatory drug clodronate: evidence for the formation in vivo of a metabolite that inhibits bone resorption and causes osteoclast and macrophage apoptosis. Arthritis Rheum 2001; 44(9): 2201–2210, https://doi.org/10.1002/1529-0131(200109)44:92201::aid-art3743.0.co;2-e.
- Lehenkari P.P., Kellinsalmi M., Näpänkangas J.P., Ylitalo K.V., Mӧnkkӧnen J., Rogers M.J., Azhayev A., Väänänen H.K., Hassinen I.E. Further insight into mechanism of action of clodronate: inhibition of mitochondrial ADP/ATP translocase by a nonhydrolyzable, adenine-containing metabolite. Mol Pharmacol 2002; 61(5): 1255–1262, https://doi.org/10.1124/mol.61.5.1255.
- Bando K., Kuroishi T., Tada H., Oizumi T., Tanaka Y., Takahashi T., Mizoguchi I., Sugawara S., Endo Y. Nitrogen-containing bisphosphonates and lipopolysaccharide mutually augment inflammation via adenosine triphosphate (ATP)-mediated and interleukin 1β (IL-1β)-mediated production of neutrophil extracellular traps (NETs). J Bone Miner Res 2021; 36(9): 1866–1878, https://doi.org/10.1002/jbmr.4384.
- Göbel A., Zinna V.M., Dell’Endice S., Jaschke N., Kuhlmann J.D., Wimberger P., Rachner T.D. Anti-tumor effects of mevalonate pathway inhibition in ovarian cancer. BMC Cancer 2020; 20(1): 703, https://doi.org/10.1186/s12885-020-07164-x.
- Dunford J.E., Kwaasi A.A., Kavanagh K.L., Rogers M.J., Oppermann U., Barnett B.B., Ebetino F.H., Russell R.G.G. Structure activity relationships of nitrogen containing bisphosphonates which induce conformational changes in farnesyl pyrophosphate synthase. Bonе 2008; 42 (Suppl 1): S71, https://doi.org/10.1016/j.bone.2007.12.129.
- Tsoumpra M.K., Muniz J.R., Barnett B.L., Kwaasi A.A., Pilka E.S., Kavanagh K.L., Evdokimov A., Walter R.L., Von Delft F., Ebetino F.H., Oppermann U., Russell R.G.G., Dunford J.E. The inhibition of human farnesyl pyrophosphate synthase by nitrogen-containing bisphosphonates. Elucidating the role of active site threonine 201 and tyrosine 204 residues using enzyme mutants. Bone 2015; 81: 478–486, https://doi.org/10.1016/j.bone.2015.08.020.
- Elmariah S. Slowing the progression of aortic stenosis: the emerging role of bisphosphonates. In: Cardiac valvular medicine. Rajamannan N.M. (editor). London: Springer-Verlag; 2013; p. 123–132, https://doi.org/10.1007/978-1-4471-4132-7_13.
- Plotkin L.I., Buvinic S., Balanta-Melo J. In vitro and in vivo studies using non-traditional bisphosphonates. Bone 2020; 134: 115–301, https://doi.org/10.1016/j.bone.2020.115301.
- Watts N.B., Diab D.L. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab 2010; 95(4): 1555–1565, https://doi.org/10.1210/jc.2009-1947.
- Rizzoli R. Long-term use of bisphosphonates in osteoporosis. Womens Health 2006; 2(2): 309–315, https://doi.org/10.2217/17455057.2.2.309.
- Aro E., Moritz N., Mattila K., Aro H.T. A long-lasting bisphosphonate partially protects periprosthetic bone, but does not enhance initial stability of uncemented femoral stems: a randomized placebo-controlled trial of women undergoing total hip arthroplasty. J Biomech 2018; 75: 35–45, https://doi.org/10.1016/j.jbiomech.2018.04.041.
- Rogers M.J., Mönkkönen J., Munoz M.A. Molecular mechanisms of action of bisphosphonates and new insights into their effects outside the skeleton. Bone 2020; 139: 115493, https://doi.org/10.1016/j.bone.2020.115493.
- Li K.Y.C. Bioprosthetic heart valves: upgrading a 50-year old technology. Front Cardiovasc Med 2019; 6: 47, https://doi.org/10.3389/fcvm.2019.00047.
- Vyavahare N., Tam H. Bioprosthetic heart valves: from a biomaterials perspective. In: Advances in heart valve biomechanics. Sacks M.S., Liao J. (editors). Cham: Springer Nature Switzerland; 2018; p. 337–382, https://doi.org/10.1007/978-3-030-01993-8_14.
- Barbarash L.S., Zhuravleva I.Yu. Bioprosthetic heart valve evolution: two decades of advances and challenges. Kompleksnye problemy serdecno-sosudistyh zabolevanij 2012; 1: 4–11.
- Mirani B., Parvin Nejad S., Simmons C.A. Recent progress toward clinical translation of tissue engineered heart valves. Can J Cardiol 2021; 37(7): 1064–1077, https://doi.org/10.1016/j.cjca.2021.03.022.
- Shemin R.J. The pursuit of optimal tissue valve durability: novel treatments. J Thorac Cardiovasc Surg 2018; 156(1): 196, https://doi.org/10.1016/j.jtcvs.2018.04.059.
- Braile-Sternieri M.C.V.B., Goissis G., Giglioti A.F., Ramirez V.D.A., Pereira N.P., Vasconcellos A., Basso-Frazzato G.G., Braile D.M. In vivo evaluation of Vivere bovine pericardium valvular bioprosthesis with a new anti-calcifying treatment. Artif Organs 2020; 44(11): E482–E493, https://doi.org/10.1111/aor.13718.
- Manji R.A., Lee W., Cooper D.K.C. Xenograft bioprosthetic heart valves: past, present and future. Int J Surg 2015; 23(Pt B): 280–284, https://doi.org/10.1016/j.ijsu.2015.07.009.
- Filová E., Staňková L., Eckhardt A., Svobodová J., Musílková J., Pala J., Hadraba D., Brynda E., Koňařík M., Pirk J., Bačáková L. Modification of human pericardium by chemical crosslinking. Physiol Res 202; 69(1): 49–59, https://doi.org/10.33549/physiolres.934335.
- Shaik T.A., Alfonso-García A., Zhou X., Arnold K.M., Haudenschild A.K., Krafft C., Leigh Griffiths L.G., Popp J., Marcu L. FLIm-guided Raman imaging to study cross-linking and calcification of bovine pericardium. Anal Chem 2020; 92(15): 10659–10667, https://doi.org/10.1021/acs.analchem.0c01772.
- Meuris B., De Praetere H., Strasly M., Trabucco P., Lai J.C., Verbrugghe P., Herijgers P. A novel tissue treatment to reduce mineralization of bovine pericardial heart valves. J Thorac Cardiovasc Surg 2018; 156(1): 197–206, https://doi.org/10.1016/j.jtcvs.2018.01.099.
- Borer J.S. Bioprosthesis failure: is calcification the only problem? J Am Coll Cardiol 2020; 76(15): 1749–1750, https://doi.org/10.1016/j.jacc.2020.08.065.
- Agathos E.A., Tomos P.I., Kostomitsopoulos N., Koutsoukos P.G. A novel anticalcification treatment strategy for bioprosthetic valves and review of the literature. J Card Surg 2019; 34(10): 895–900, https://doi.org/10.1111/jocs.14151.
- Kiesendahl N., Schmitz C., Von Berg A., Menne M., Schmitz-Rode J., Steinseifer U. In vitro calcification of bioprosthetic heart valves: investigation of test fluids. Ann Biomed Eng 2020; 48(1): 282–297, https://doi.org/10.1007/s10439-019-02347-5.
- D’Alessandro C., Dimopoulos A., Andriopoulou S., Messaris G.A.T., Korossis S., Koutsoukos P., Mavrilas D. In vitro calcification studies on bioprosthetic and decellularized heart valves under quasi-physiological flow conditions. Bio-Des Manuf 2020; 4: 10–21, https://doi.org/10.1007/s42242-020-00110-7.
- D’Alessandro C.C., Komninou M.A., Badria A.F., Korossis S., Koutsouko P., Mavrilas D. Calcification assessment of bioprosthetic heart valve tissues using an improved in vitro model. IEEE Trans Biomed Eng 2020; 67(9): 2453–2461, https://doi.org/10.1109/tbme.2019.2963043.
- Luo Y., Huang S., Ma L. A novel detergent-based decellularization combined with carbodiimide crosslinking for improving anti-calcification of bioprosthetic heart valve. Biomed Mater 2021; 16(4): 045022, https://doi.org/10.1088/1748-605x/ac0088.
- Park C.S., Kim Y.J., Lee J.R., Lim H.G., Chang J.H., Jeong S., Kwon N. Anticalcification effect of a combination of decellularization, organic solvents and amino acid detoxification on glutaraldehyde-fixed xenopericardial heart valves in a large-animal long-term circulatory model. Interact Cardiovasc Thorac Surg 2017; 25(3): 391–399, https://doi.org/10.1093/icvts/ivx131.
- Jorge-Herrero E., Garcia Paez J.M., Del Castilo-Olivares Ramos J.L. Tissue heart valve mineralization: review of calcification mechanisms and strategies for prevention. J Appl Biomater Biomech 2005; 3(2): 67–68.
- Schoen F.J., Levy R.J. Calcification of tissue heart valve substitutes: progress toward understanding and prevention. Ann Thorac Surg 2005; 79(3): 1072–1080, https://doi.org/10.1016/j.athoracsur.2004.06.033.
- Lee C.H. Physiological variables involved in heart valve substitute calcification. Expert Opin Biol Ther 2009; 9(8): 1031–1042, https://doi.org/10.1517/14712590903085091.
- Munnelly A., Schoen F., Vyavahare N. Biomaterial calcification: mechanisms and prevention. In: Degradation of implant materials. Eliaz N. (editor). New York: Springer; 2012; p. 359–392, https://doi.org/10.1007/978-1-4614-3942-4_14.
- Demer L.L., Tintut Y. Heart valve calcification. In: Principles of heart valve engineering. Kheradvar A. (editor). Cambridge, Massachusetts: Academic Press; 2019; p. 307–319, https://doi.org/10.1016/b978-0-12-814661-3.00011-3.
- Schoen F.J., Levy R.J. Bioprosthetic heart valve calcification: clinicopathologic correlations, mechanisms, and prevention. In: Contemporary cardiology. Aikawa E., Hutcheson J.D. (editors). Cham: Humana Press; 2020; p. 183–215, https://doi.org/10.1007/978-3-030-46725-8_9.
- Schoen F.J., Levy R.J., Tam H., Vyavahare N. Pathological calcification of biomaterials. In: Biomaterials science. Wagner W.R., Sakiyama-Elbert S.E., Zhang G., Yaszemski M.J. (editors). Cambridge, Massachusetts: Academic Press; 2020; p. 973–994, https://doi.org/10.1016/b978-0-12-816137-1.00065-9.
- Hirsch D., Schoen F.J., Levy R.J. Effects of metallic ions and diphosphonates on inhibition of pericardial bioprosthetic tissue calcification and associated alkaline phosphatase activity. Biomaterials 1993; 14(5): 371–377, https://doi.org/10.1016/0142-9612(93)90057-9.
- Golomb G., Dixon M., Smith M.S., Schoen F.J., Levy R.J. Controlled-release drug delivery of diphosphonates to inhibit bioprosthetic heart valve calcification: release rate modulation with silicone matrices via drug solubility and membrane coating. J Pharm Sci 1987; 76(4): 271–276, https://doi.org/10.1002/jps.2600760402.
- Golomb G., Dixon M., Smith M.S., Schoen F.J., Levy R.J. Inhibition of bioprosthetic heart valve calcification by sustained local delivery of Ca and Na diphosphonate via controlled release matrices. ASAIO Trans 1986; 32(1): 587–590, https://doi.org/10.1097/00002216-198609000-00045.
- Sovány T., Csüllög A., Benkő E., Regdon G. Jr., Pintye-Hódi K. Comparison of the properties of implantable matrices prepared from degradable and non-degradable polymers for bisphosphonate delivery. Int J Pharm 2017; 533(2): 364–372, https://doi.org/10.1016/j.ijpharm.2017.07.023.
- Balas F., Manzano M., Horcajada P., Vallet-Regí M. Confinement and controlled release of bisphosphonates on ordered mesoporous silica-based materials. J Am Chem Soc 2006; 128(25): 8116–8117, https://doi.org/10.1021/ja062286z.
- Synetos A., Toutouzas K., Drakopoulou M., Koutagiar I., Benetos G., Kotronias R., Anousakis-Vlachochristou N., Latsios G., Karanasos A., Agrogiannis G., Metaxas M., Stathogiannis K., Papanikolaou A., Georgakopoulos A., Pianou N., Tsiamis E., Patsouris E., Papalois A., Cokkinos D., Anagnostopoulos C., Tousoulis D. Inhibition of aortic valve calcification by local delivery of zoledronic acid — an experimental study. J Cardiovasc Transl Res 2018; 11(3): 192–200, https://doi.org/10.1007/s12265-018-9802-4.
- Santos L.L., Cavalcanti T.B., Bandeira F.A. Vascular effects of bisphosphonates — a systematic review. Clin Med Insights Endocrinol Diabetes 2012; 5: 47–54, https://doi.org/10.4137/cmed.s10007.
- Donato M., Ferri N., Lupo M.G., Faggin E., Rattazzi M. Current evidence and future perspectives on pharmacological treatment of calcific aortic valve stenosis. Int J Mol Sci 2020; 21(21): 8263, https://doi.org/10.3390/ijms21218263.
- Cutini P.H., Rauschemberger M.B., Sandoval M.J., Massheimer V.L. Vascular action of bisphosphonates: in vitro effect of alendronate on the regulation of cellular events involved in vessel pathogenesis. J Mol Cell Cardiol 2016; 100: 83–92, https://doi.org/10.1016/j.yjmcc.2016.08.017.
- Dayanand P., Sandhyavenu H., Dayanand S., Martinez J., Rangaswami J. Role of bisphosphonates in vascular calcification and bone metabolism: a clinical summary. Curr Cardiol Rev 2018; 14(3): 192–199, https://scite.ai/reports/10.2174/1573403x14666180619103258.
- Elnashar M.M. Immobilized molecules using biomaterials and nanobiotechnology. J Biomater Nanobiotechnol 2010; 1(1): 61–77, https://doi.org/10.4236/jbnb.2010.11008.
- Fleisch H., Russell R.G., Bisaz S., Mühlbauer R. Influence of diphosphonates on the deposition and dissolution of ccalcium phosphate in vitro and in vivo. Helv Physiol Pharmacol Acta 1968; 26(3): CR345–CR346.
- Dewanjee M.K., Solis E., Lanker J., Mackey S.T., Lombardo G.M., Tidwell C., Ellefsen R.D., Kaye M.P. Effect of diphosphonate binding to collagen upon inhibition of calcification and promotion of spontaneous endothelial cell coverage on tissue valve prostheses. ASAIO Trans 1986; 32(1): 24–29.
- Dewanjee M.K. Treatment of collagen tissue with glutaraldehyde and aminophosphonate calcification inhibitor. Patent US 4553974. 1985.
- Webb C.L., Phelps L.L., Schoen F.J., Levy R.J. Aminodiphosphonate or AI preincubation inhibits calcification of aortic homografts in the rat subdermal model. ASAIO Trans 1988; 34(3): 851–854.
- Johnston T.P., Schoen F.J., Levy R.J. Prevention of calcification of bioprosthetic heart valve leaflets by Ca2+ diphosphonate pretreatment. J Pharm Sci 1988; 77(9): 740–744, https://doi.org/10.1002/jps.2600770903.
- Webb C.L., Benedict J.J., Schoen F.J., Linden J.A., Levy R.J. Inhibition of bioprosthetic heart valve calcification with aminodiphosphonate covalently bound to residual aldehyde groups. Ann Thorac Surg 1988; 46(3): 309–316, https://doi.org/10.1016/s0003-4975(10)65932-2.
- Webb C.L., Schoen F.J., Levy R.J. Covalent binding of aminopropanehydroxydiphosphonate to glutaraldehyde residues in pericardial bioprosthetic tissue: stability and calcification inhibition studies. Exp Mol Pathol 1989; 50(3): 291–302, https://doi.org/10.1016/0014-4800(89)90039-7.
- Nimni M.E., Ertl D., Villanueva J., Nimni B.S. Inhibition of ectopic calcification of glutaraldehyde crosslinked collagen and collagenous tissues by a covalently bound diphosphonate (APD). Am J Cardiovasc Pathol 1990; 3(3): 237–245.
- Levy R.J., Qu X., Underwood T., Trachy J., Schoen F.J. Calcification of valved aortic allografts in rats: effects of age, crosslinking, and inhibitors. J Biomed Mater Res 1995; 29(2): 217–226, https://doi.org/10.1002/jbm.820290212.
- Savino S., Toscano A., Purgatorio R., Profilo E., Laghezza A., Tortorella P., Angelelli M., Cellamare S., Scala R., Tricarico D., Marobbio C.M.T., Perna F., Vitale P., Agamennone M., Dimiccoli V., Tolomeo A., Scilimati A. Novel bisphosphonates with antiresorptive effect in bone mineralization and osteoclastogenesis. Eur J Med Chem 2018; 158: 184–200, https://doi.org/10.1016/j.ejmech.2018.08.044.
- Widler L., Jaeggi K.L., Glatt M., Müller K., Bachmann R., Bisping M., Born A.R., Cortesi R., Guiglia G., Jeker H., Klein R., Ramseier U., Schmid J., Schreiber G., Seltenmeyer Y., Green J.R. Highly potent geminal bisphosphonates. From pamidronate disodium (Aredia) to zoledronic acid (Zometa). J Med Chem 2002; 45(17): 3721–3738, https://doi.org/10.1021/jm020819i.
- Ishida K., Ashizawa N., Matsumoto K., Kobashi S., Kurita N., Shigematsu T., Iwanaga T. Novel bisphosphonate compound FYB-931 preferentially inhibits aortic calcifcation in vitamin D3-treated rats. J Bone Miner Metab 2019; 37(5): 796–804, https://doi.org/10.1007/s00774-019-00987-0.
- Zhuravleva I.Y., Polienko Y.F., Karpova E.V, Timchenko T.P., Vasilieva M.B., Baratova L.A., Shatskaya S.S., Kuznetsova E.V., Nichay N.R., Beshchasna N., Bogachev-Prokophiev A.V. Treatment with bisphosphonates to mitigate calcification of elastin-containing bioprosthetic materials. J Biomed Mater Res A 2020; 108(7): 1579–1588, https://doi.org/10.1002/jbm.a.36927.
- Jin W., Guo G., Chen L., Lei Y., Wang Y. Elastin stabilization through polyphenol and ferric chloride combined treatment for the enhancement of bioprosthetic heart valve anticalcification. Artif Organs 2018; 42(11): 1062–1069, https://doi.org/10.1111/aor.13151.
- Zhuravleva I.Y., Nichay N.R., Kulyabin Y.Y., Timchenko T.P., Korobeinikov A.A., Polienko Y.F., Shatskaya S.S., Kuznetsova E.V., Voitov A.V., Bogachev-Prokophiev A.V., Karaskov A.M. In search of the best xenogeneic material for a paediatric conduit: an experimental study. Interact Cardiovasc Thorac Surg 2018; 26(5): 738–744, https://doi.org/10.1093/icvts/ivx445.
- Nichay N.R., Zhuravleva I.Y., Kulyabin Y.Y., Timchenko T.P., Voitov A.V., Kuznetsova E.V., Soynov I.A., Zubritskiy A.V., Bogachev-Prokophiev A.V., Karaskov A.M. In search of the best xenogeneic material for a paediatric conduit: an analysis of clinical data. Interactive Interact Cardiovasc Thorac Surg 2018; 27(1): 34–41, https://doi.org/10.1093/icvts/ivy029.
- Hendriks M., Everaerts F., Verhoeven M. Bioprostheses and its alternative fixation. J Long Term Eff Med Implants 2017; 27(2–4): 137–157, https://doi.org/10.1615/jlongtermeffmedimplants.v27.i2-4.40.
- Rezvova M.A., Ovcharenko E.A., Glushkova T.V., Kudryavtseva Yu.A., Barbarash L.S. Evaluation of calcification resistance of xenopericardium treated with polyhydroxy compounds. Vestnik transplantologii i iskusstvennyh organov 2021; 23(1): 75–83, https://doi.org/10.15825/1995-1191-2021-1-75-83.
- Yu T., Yang W., Zhuang W., Tian Y., Kong Q., Chen X., Li G., Wang Y. A bioprosthetic heart valve cross-linked by a non-glutaraldehyde reagent with improved biocompatibility, endothelialization, anti-coagulation and anti-calcification properties. J Mater Chem B 2021; 9(19): 4031–4038, https://doi.org/10.1039/d1tb00409c.










