Biological and Prognostic Role of Tumor Size (T1a, T1b, T1c) in Stage I Breast Cancer (Experience of International Cooperation)
The aim of the investigation was to study shared distribution of tumors T1a, T1b and T1c in two independent female populations: in the country with National breast cancer screening program (the Netherlands) and in the country with voluntary mammographic screening program (Russia), and assess biological and prognostic value of tumor size for the risk of further disease progression and cancer-related mortality.
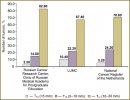
Materials and Methods. We studied stage I breast cancer (T1N0M0) heterogeneity in Russian and Dutch female population. The study involved Russian women who had undergone radical treatment in N.N. Blokhin Russian Cancer Research Center of Russian Academy of Medical Science and Clinic of Russian Medical Academy for Postgraduate Education (n=1341), Dutch women who had received treatment in LUMC (n=553) and the patients included in National Cancer Register of the Netherlands (n=22196).
Results. Percentage of tumors <10 mm (T1a and T1b) in Dutch women is significantly higher (to 34%) compared with that in Russian women (17.1%) that can be explained by the differences in breast cancer screening in these countries. Stage I breast cancer is a heterogeneous group with a favorable course, if microcarcinomas are <5 mm, and more aggressive — in tumors T1b and T1c. Only microcarcinomas T1a have a favorable biological “portrait” (high percentage of luminal А-subtype tumors with low anaplasia degree) that has an impact on long-term treatment results (minimum recurrence rate and mortality rate and best long-term survival rate). Biological characteristics of tumors T1b and T1c are more aggressive and have higher percentage of ductal breast cancer with luminal В-subtype and triple negative cancer immunophenotype that significantly worsens the disease prognosis.
- GLOBOСAN 2012. http://globocan.iarc.fr.
- Saika K., Sobue T. Cancer statistics in the world. Gan To Kagaku Ryoho 2013 Dec; 40(13): 2475–2480.
- Thomas B.A., Price J.L., Boulter P.S., Gibbs N.M. The first three years of the Guildford Breast Screening Project. Recent Results Cancer Res 1984; 90: 195–199.
- Goin J.E., Haberman J.D., Linder M.K., Lambird P.A. Analysis of mammography: a blind interpretation of BCDDP radiographs. Radiology 1983 Aug; 148(2): 393–396.
- Brisson J., Morrison A.S., Khalid N. Mammographic parenchymal features and breast cancer in the breast cancer detection demonstration project. J Natl Cancer Inst 1988 Dec 7; 80(19): 1534–1540, http://dx.doi.org/10.1093/jnci/80.19.1534.
- Smart C.R., Byrne C., Smith R.A., et al. Twenty-year follow-up of the breast cancers diagnosed during the Breast Cancer Detection Demonstration Project. CA Cancer J Clin 1997 May–Jun; 47(3): 134–149.
- Tabar L., Yen M.F., Vitak B., et al. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet 2003; 361: 1405–1410, http://dx.doi.org/10.1016/S0140-6736(03)13143-1.
- Gotzsche P.C., Olsen O. Is screening for breast cancer with mammography justifiable? Lancet 2000; 355: 129–134, http://dx.doi.org/10.1016/S0140-6736(99)06065-1.
- Health Quality Ontario. Screening mammography for women aged 40 to 49 years at average risk for breast cancer: an evidence-based analysis. Ont Health Technol Assess Ser 2007; 7(1): 1–32.
- Weisstock C.R., Rajapakshe R., Bitgood C., et al. Assessing the breast cancer risk distribution for women undergoing screening in British Columbia. Cancer Prev Res 2013 Oct; 6(10): 1084–1092, http://dx.doi.org/10.1158/1940-6207.CAPR-13-0027.
- Mohammed Z.M., McMillan D.C., Edwards J., Mallon E., Doughty J.C., Orange C., Going J.J. The relationship between lymphovascular invasion and angiogenesis, hormone receptors, cell proliferation and survival in patients with primary operable invasive ductal breast cancer. BMC Clin Pathol 2013 Nov 25; 13(1): 31, http://dx.doi.org/10.1186/1472-6890-13-31.
- Uchida N., Suda T., Ishiguro K. Effect of chemotherapy for luminal a breast cancer. Yonago Acta Med 2013 Jun; 56(2): 51–56.
- Rouanet P., Roger P., Rousseau E., Thibault S., Romieu G., Mathieu A., Cretin J., Barneon G., Granier M., Maran-Gonzalez A., Daures J.P., Boissiere F., Bibeau F. HER2 overexpression a major risk factor for recurrence in pT1a-bN0M0 breast cancer: results from a French regional cohort. Cancer Med 2014 Jan 10, http://dx.doi.org/10.1002/cam4.167.
- Comen E.A., Norton L., Massague J. Breast cancer tumor size, nodal status, and prognosis: biology trumps anatomy. J Clinical Oncology 2011; 2619–2622, http://dx.doi.org/10.1200/JCO.2011.36.1873.










